Alarming rise in child deaths from antimicrobial resistance
New research reveals over 3 million children died globally from AMR-related infections in 2022, with particular concerns about increasing use of critical antibiotic classes.
A landmark study presented at ESCMID Global 2025 has revealed the devastating impact of antimicrobial resistance (AMR) on children worldwide, with more than 3 million paediatric deaths attributed to AMR-related infections in 2022 alone.
The research, presented on 13 April 2025, highlights an urgent need for coordinated regional and global strategies to control paediatric AMR, particularly in high-burden regions such as South-East Asia and Africa.
Regional impacts and antibiotic use patterns
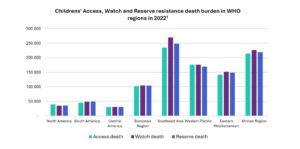
The study found that in 2022, more than 752,000 children in Southeast Asia and 659,000 children in Africa died of AMR-associated complications. Many of these deaths were linked to the increased use of World Health Organization (WHO) classified ‘Watch’ antibiotics (drugs with a high risk of resistance) and ‘Reserve’ antibiotics (last-resort treatments for severe, multidrug-resistant infections).
Between 2019 and 2021, the use of Watch antibiotics increased by 160% in Southeast Asia and 126% in Africa. During the same period, the use of Reserve antibiotics rose by 45% in Southeast Asia and 125% in Africa.
Of the more than 3 million global paediatric deaths, approximately 2 million were associated with the use of Watch and Reserve antibiotics.
“While the rise in use of Watch and Reserve antibiotics may be necessary in response to the concurrent rise in drug-resistant infections, the sharp rise in use of these drugs presents several serious long-term risks”, commented Professor Joseph Harwell, study co-author. “Their increased use, especially without careful oversight, elevates the risk of resistance and limits future treatment options. If bacteria develop resistance to these antibiotics, there will be few, if any, alternatives for treating multidrug-resistance infections.”
Contributing factors in resource-limited settings
The research identified several factors contributing to the severity of AMR in low- and middle-income countries, including:
- Overcrowded healthcare facilities
- Poor sanitation
- Weak infection prevention measures
- Lack of diagnostic tools leading to antibiotic overuse
- Insufficient surveillance systems and antimicrobial stewardship programmes
“Rising resistance to Watch and Reserve antibiotics will ultimately lead to higher treatment failure,” said Professor Harwell. “Mortality rates, which are already alarmingly high, will continue to rise significantly, particularly in low- and middle-income countries where access to alternative treatments and advanced medical interventions may be limited.”
Calls for urgent action
The researchers emphasise the need for immediate and coordinated action, including:
- Implementation of hospital-based antimicrobial stewardship programmes in all paediatric healthcare facilities
- Improved age classifications in surveillance data
- Development of national guidelines to ensure routine surveillance informs antibiotic use
- Global and national surveillance adopting a ‘One Health’ approach
“Addressing this issue requires urgent and coordinated action at both the regional and global levels. Global and national surveillance on AMR must adopt a ‘One Health’ approach, with cost-effective systems that can inform treatment guidelines and measure the impact of control interventions,” Professor Harwell stated.
AMR poses a particularly critical threat to children, who are highly vulnerable to infections, and whose access to new antibiotic formulations is often limited due to development delays.
The study incorporated data from the Pfizer ATLAS programme provided through the Vivli platform, along with WHO’s GLASS on antibiotic use, the World Bank data on demographics, and IHME mortality data.
Reference:
Hu, Y., & Harwell, J. (2025). Global Trends and Impact of Antimicrobial Resistance in Paediatric Populations: An Analysis Using WHO AWaRe Classification and Priority Pathogens. Oral presentation. ESCMID Global 2025.