Improved tools to diagnose venom allergies
Bee and wasp venom allergy is a potentially life-threatening condition and diagnostic errors can therefore have serious consequences. Currently, the diagnosis of allergy to stinging insects relies on patient case history and quantification of specific IgE antibodies and skin prick testing to identify the responsible insect. However, the diagnosis can sometimes be problematic as patients may have very low levels of specific IgE and also because many patients show positive test results to several venom species. Moreover it is often difficult for the patient to identify the offending insect. Component based specific IgE testing helps to increase the sensitivity of testing as well as to resolve which stinging insect species the patient is sensitized to. By applying these new component-specific IgE tests and including testing for serum tryptase, the certainty in identifying patients that will benefit from relevant and safe venom immunotherapy treatment increases greatly.
by Magnus Borres, MD, PhD, MPH
Background
Venoms from stinging insects such as bees and wasps (Hymenoptera) can induce anaphylaxis in susceptible people, and stinging insects are the second most common cause of anaphylaxis in Europe and USA (prevalence of 0.3 to 7.5% in Europe). Most of the severe and fatal reactions to insect stings in Europe are caused by members of the Vespidae family – commonly known as wasps. In contrast to many other IgE mediated allergic reactions, venom allergies may arise very unexpectedly as they can affect also individuals that do not have a genetic pre-disposition to make IgE antibodies.
The reactions elicited by a bee or wasp sting can range from mild/local immediate reactions, to larger often late local reactions up to immediate systemic reactions, eventually leading into life threatening conditions requiring emergency treatment.
Markers and risk factors in venom allergies
The presence of specific IgE antibodies to venoms supports the diagnosis of an allergic reaction. In many patients however, the levels are low and there is no direct correlation between the levels of specific IgE antibodies and the risk for reactions. In fact, it is not uncommon that severe reactions occur in patients with very low or sometimes even undetectable venom-specific IgE levels. This exemplifies the need for highly sensitive diagnostic tests that can detect and quantify very low specific IgE levels.
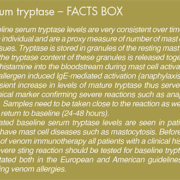
The risk of developing severe reactions after a Hymenoptera sting is dependent on several factors, such as the patient’s history of previous reactions, serum tryptase levels, age and specific IgE-sensitization. People who have already suffered from severe systemic reactions due to stings are predisposed for future reactions – up to 80% will develop severe reactions following a subsequent sting. However, in 50% of the fatal cases no previous systemic reaction has occurred. Serum tryptase is an important marker for evaluating the risk for systemic reactions, where elevated baseline tryptase levels indicate a higher risk for severe anaphylactic reactions. Approximately a fourth of patients who experience severe venom reactions have elevated baseline levels of this marker. The risk for severe reaction to venom stings also increases with age, and is higher in adults than in children and adolescents. This may be explained by an increased number of mast cells in addition to other contributing clinical conditions in older people.
Identify the little beast!
For patients who are highly allergic to insect stings the treatment option is to undergo venom immunotherapy (VIT) aiming at inducing tolerance. For selecting the most effective treatment, correct identification of the Hymenoptera species that causes reactions in the patient is crucial. This is however not trivial as many patients do not know what insect stung them, and as approximately 60% of the patients show up positive to both bee and wasp in venom extract-based tests.
Diagnostic in vitro tests in venom allergies
Patient history forms the basis in diagnosing a venom allergy and specific IgE antibody test results can support the doctor in the diagnosis and in choosing the appropriate treatment. Whether the reaction in a patient is IgE mediated or not needs to be established. This is usually done by in vitro testing for specific IgE and/or skin prick testing, but as many as 10-20% who seek medical care for sting-induced reactions are negative in these extract-based tests. The reason may be that the reaction was due to another pathogenic mechanism than an allergic reaction, or it could have been caused by an underlying mast cell disease. When using conventional extract based test, which due to the preparation procedure may be low in content of certain allergenic proteins, the sensitivity may not be high enough to pick up certain sensitizations. In addition patients reacting for the first time to a sting may initially have levels of venom-specific IgE below the detection limit.
On the other hand, it is common that patients appear to be sensitized to both bee and wasp venoms when using extractbased specific IgE tests, even in cases when proven non-reactive to one of the species. Diagnostic tests capable of discriminating between clinically relevant and irrelevant sensitizations, while reliably detecting true co-sensitization to both species greatly improves proper diagnosis and selection of therapeutic interventions.
There has thus been a need to increase both the sensitivity to detect low levels of IgE antibodies and the specificity to distinguish between sensitization to different Hymenoptera species. Recently this has become possible through the introduction of component-resolved diagnostics, or molecular allergology.
What is molecular allergology?
Molecular allergology allows the measurement of specific IgE antibodies to single, pure allergen molecules, thereby helping to identify the exact allergenic molecule (component) that a patient is sensitized to. All allergen sources contain several allergenic molecules, and the ability to produce these by recombinant means and assay them individually greatly increases the precision of specific IgE measurements. Using this component-resolved testing it is possible to discriminate between species-specific sensitizations, where the patient is genuinely sensitized to the allergen source, and sensitizations due to cross-reactivity. Cross-reactivity occurs when antibodies directed against one molecule cross-recognize a very similar but yet distinct protein. Such cross-reactivity may arise due to high similarity between some components in bees and wasps, but may also be caused by carbohydrate structures (CCDs) on proteins in plants and invertebrates. CCD antibodies do not cause symptoms and are thus clinically irrelevant, but may confuse test results greatly. Recombinant components used in molecular allergology are free of CCD structures and are therefore very specific. In addition, tests that identify antibodies to CCD are available to further increase diagnostic accuracy.
Molecular allergology improves the allergy diagnosis
Results from extract-based tests give the first, although crude answers that guide the diagnosis, while further analyses using component-based testing take the diagnosis to completely new levels by offering improved test sensitivity, resolving ambiguous extract test results and guiding the selection of optimal treatment. In cases where the patient has a convincing history of bee or wasp allergy, but extract -based tests turn out negative, allergen component testing offers increased sensitivity to detect relevant sensitizations. These tests contain only one single pure allergen component therefore the sensitivity to detect antibodies directed to this unique protein is increased as compared to extract-based tests. However the strength of the extract-based test is that they do contain all relevant allergenic proteins in the allergen source, including minor allergens.
Component-based testing enables the discrimination between true co-sensitization and sensitization due to cross-reactivity. Extract-based test results may indicate sensitization to both bee and wasp venoms, but using component testing it is possible to investigate if these sensitizations are clinically irrelevant or truly suggest allergy to both species. The recombinant markers for bee (Api m 1), common wasp (Ves v 1 and Ves v5) and/or paper wasp (Pol d 5) should be used to determine unambiguously if the sensitization is species-specific or not. CCD-antibodies can also give rise to double positive test results in the absence of specific Hymenoptera venom sensitization since these antibodies often are induced by grass sensitization.
When extract-based test turn out positive to either bee or wasp only, there is little questioning about what species that patient reacts to. Even though this indicates a true Hymenoptera venom sensitization, additional testing with component-based tests can confirm if the patient is sensitized to a major allergen in the relevant species. Venom immunotherapy treatment may be more effective in patients who are sensitized to these major allergens.
New diagnostic tools in Hymenoptera venom allergy are now available for clinicians
The recent development of IgE tests against species-specific allergen components in Hymenoptera venom allergy offers diagnostic tools that greatly improve the ability to differentiate between sensitization to bees and wasp, and helps in discriminating between clinically relevant and irrelevant sensitizations.
Identification of which molecules that triggers the severe reaction is of vital importance for the clinician when considering venom immunotherapy. The combined use of venom components and Tryptase optimize the diagnosis and management of patients with a suspicion of venom allergy. Currently only Thermo Fisher Scientific, formerly known as Phadia, Uppsala, Sweden, have both tryptase and allergen component test available on the same technology platform.
The author
By Magnus Borres, MD, PhD, MPH
Pediatric Allergist, Uppsala University Hospital, Uppsala, Sweden
Medical Director, ImmunoDiagnostics, Thermo Fisher Scientific, Uppsala, Sweden