Managing chronic disease: do clinical labs hold the key ?
Chronic diseases are placing an increasingly heavy burden on the healthcare systems of both development and emerging countries. Together with renewed prevention strategies based on systematic and coordinated approaches, clinical laboratories will have an essential role to play with the advent of new biomarkers and the development of e-health systems.
Chronic diseases are acknowledged to be one of the biggest challenges for healthcare systems. Traditionally, chronic diseases were non-communicable. Using World Health Organization (WHO) data [1], they consisted of four major groups – cardiovascular diseases, cancers, chronic respiratory diseases and diabetes, as well as some neuropsychiatric disorders and arthritis. More recently, an increase in survival rates for infectious and genetic diseases has led to expanding the definition to certain communicable diseases (such as HIV/AIDS) as well as genetic disorders like cystic fibrosis.
Attention to chronic diseases has been growing, largely due to three factors:
1. Ageing populations.
2. Early detection, or ‘secondary prevention’.
3. E-health – the possibility offered by sophisticated at-home monitoring and timely treatment.
Ageing populations
The elderly are far more susceptible to chronic disease. In the US, some 10% of the beneficiaries of Medicare, almost all with chronic disease, account for three-quarters of its budget. [2] Per capita spending is 3-10 times more for older adults with chronic diseases than those without. [3] In Europe, the EU Council has noted the “enormous burden” posed by chronic diseases and also warned that the next decade (2011-2020) will see this grow further due to an ageing population. [4]
Early detection
The early detection of chronic disease has been revolutionized by virtue of innovative and ever-faster diagnostic techniques in clinical laboratories. Clinical laboratories have, for some years, taken the lead in reducing the gap between the evolution of a chronic disease and interventional treatment, both at home and in the hospital.
In 2007, a report by the influential Milken Institute think-tank made a powerful argument to include prevention and early detection, rather than treatment alone, in the US debate on funding healthcare. The Milken report was titled ‘An Unhealthy America: The Economic Burden of Chronic Disease’. [5] It was one of the most ambitious attempts to quantify the reduction in case burden that could be achieved by such strategic reorientation: a drop by as many as 40 million cases of chronic diseases in the year 2023, in the US alone. At the time of the report’s launch, former US Surgeon General Richard Carmona noted the biggest problem with the present healthcare system was that it waited for people to get sick and then treated them at high cost.
The story is similar in Europe. Though EU-wide statistics do not yet exist, in the UK, half of hospital bed day use is accounted for by only 2.7% of all medical conditions, most of which are chronic diseases. [6] The EU Commission has called for technology-driven strategies to permit both early detection and timely monitoring of chronic disease – and do this in the context of healthy ageing.
As in the US, much European thinking about managing the burden of chronic disease involves e-Health, especially in the context of structured programmes of home care for patients. In January 2007, a major EU Commission study called “Healthy Ageing: Keystone for a Sustainable Europe” [7] approvingly highlighted a Swedish program called ‘Preventive Home Visits’ as leading to both a decrease in GP visits and lower mortality. It called for promoting and using such best-of-class practices across the EU.
E-health and clinical laboratories
All such plans essentially consist of remote acquisition of patient data using lower skilled and mobile personnel. They transfer the data in real- or near real-time for remote interpretation at a clinical laboratory, followed by consultation with a physician (e.g to modify dosage/change medicines), or to transfer the patient for intervention at a hospital.
The role of the clinical laboratory in e-Health is already advanced in telepathology. Though some telepathology efforts have aimed at remote manipulation of diagnostic equipment, the more proven approach has been to transmit images from a slide. Such systems have been in use since the mid-1990s, especially in sparsely populated areas such as parts of Canada and the north-western US, and in Norway and Sweden. France’s RESINTEL was, however, one of the first systems to establish that telepathology was at least as reliable as a physical slide examination, in a transatlantic pilot project. [8]
The largest application for telepathology has so far been in cytology. Nevertheless, microbiologists have been remotely interpreting gram stains, and hematologists have reported success with blood films.
Biomarkers: promises and challenges
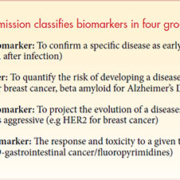
The next frontier is likely to be biomarkers – pre-symptomatic signals of early disease states, detectable in blood/serum. In 2011, an article by 61 healthcare experts from Europe, the US, Brazil, Russia, India, China and some other countries called for a systemic approach to combat chronic disease, with a roadmap “for predictive, preventive, personalized and participatory (P4) medicine.” [9] The core of the proposal is to systematically identify biomarkers, which would then (progressively) be used to chart out a matrix of co-morbidities, disease severity and progression – including the critical trigger signals which predict the occurrence of abrupt transitions in the stages of a chronic disease.
The authors of the above paper cite an in-depth study on the clinical impact of telemedicine in four major chronic diseases – diabetes, asthma, heart failure and hypertension, [10] and propose that continuous monitoring of individual clinical histories and their development would be a key source of primary data, to build up a robust and extensive knowledge management infrastructure.
The role of clinical laboratories in much of the above system – from biomarker discovery to the monitoring of patients – is evident. At the moment, tests on the bulk of approved biomarkers (such as Oncotype DX and Trofile) are conducted in large reference laboratories. However, a great deal of research is also being directed at tests for use at home or at point-of-care; for example, CRP (C-reactive protein) and the hormone prolactonin are biomarkers which differentiate between bacterial and viral pneumonia in less than an hour, and reduce the use of precautionary antibiotics.
Nevertheless, there is still some way to go before biomarkers and systemic/personal approaches to medication and treatment of chronic disease become commonplace. Most barriers are regulatory [see box on this page], and are a consequence of the relative novelty of biomarkers – and their potentially sweeping impact.
In the light of this, the challenge for clinical laboratories will be to develop acceptable technical standards for the use of biomarkers, jointly with regulators and manufacturers. Clearly, given the massive challenge posed by chronic diseases in the decades ahead, any serious solution will have to involve a combination of biomarker-based personalized medicine, at-home care and clinical laboratories.
References
1. http://www.who.int/nmh/Actionplan-PC-NCD-2008.pdf
2. Berk ML, Monheit AC. The Concentration of Health Expenditures: An Update. HealthAffairs 1992; 11 (4): 145–149.
3. Fishman P, et al. Chronic Care Costs in Managed Care. Health Affairs 1997; 16 (3): 239–247.
4. http://www.consilium.europa.eu/uedocs/cms_Data/docs/pressdata/en/lsa/118282.pdf
5. http://www.milkeninstitute.org/healthreform/pdf/AnUnhealthyAmericaExecSumm.pdf
6. Chronic Disease management – a compendium of information, UK Department of Health, May 2004
7. http://ec.europa.eu/health/archive/ph_information/indicators/docs/healthy_ageing_en.pdf
8. http://pubmedcentralcanada.ca/pmcc/articles/PMC2579163/pdf/procascamc00009-0625.pdf
9. http://genomemedicine.com/content/3/7/43#B46
10. Pare G, Moqadem K, Pineau G, St-Hilaire C. Clinical effects of home telemonitoring in the context of diabetes, asthma, heart failure and hypertension: a systematic review. J Med Internet Res 2010 (12:e21).
11. http://ec.europa.eu/research/health/pdf/biomarkers-for-patient-stratification_en.pdf
12. http://www.phgfoundation.org/file/3998/