Phage-displayed peptides as novel reagents for norovirus detection
Current methods for detecting noroviruses (NoVs) have significant limitations in sensitivity and feasibility for use in remote locations. Our group recently identified phage-displayed peptides with specific binding to NoVs and sensitivity comparable to that of existing antibodies. These reagents can be easily optimized by mutagenesis and represent promising diagnostic tools.
by Amy M. Hurwitz, Prof. Robert L. Atmar and Prof. Timothy G. Palzkill
Norovirus infection and diagnosis
Each year, norovirus (NoV) infections cause approximately 267 million new cases of gastroenteritis and 200,000 deaths worldwide [1]. Infection spreads rapidly in areas of close human contact, such as cruise ships and hospitals, and is treated only by rehydration, as no antiviral therapy currently exists. An infectious dose estimated to be as low as 18 virions and high environmental stability contributed to classification of NoVs as a category B biodefense agent in the U.S. Therefore, rapid, accurate and highly sensitive diagnosis is important for outbreak recognition and control, and also to guide physicians in patient management. The potential health and economic consequences that may be ameliorated by early NoV detection have led to a high demand for optimized detection reagents that can be used to develop reliable diagnostic assays with minimal requirements for expensive, bulky equipment or technical training.
NoVs are divided into six different genogroups (GI–GVI) based on the amino acid sequence of the major capsid protein (VP1). These are organized further into more than 30 genotypes, and finally into numerous strains or variants [2]. The VP1 protein assembles to form an icosahedral shell with an inner shell (S) domain and outer protruding (P) domain. The P domain is on the virus surface and is the most accessible, while the S domain has the highest sequence conservation across different strains. Given the ability of NoVs to evolve rapidly to result in novel or recombinant strains, continual optimization of detection reagents may be necessary in order to recognize the majority of human-infecting strains. Strains classified into GI and GII are most relevant for human infections, and thus the focus for diagnostic assay development efforts.
Current diagnostic methods and their limitations
Methods used currently for the diagnosis of norovirus infection are far from ideal as they exhibit several limitations that hinder their use for individual patient diagnoses or in rural and developing locations. The gold standard for diagnosis is reverse transcriptase (RT)-PCR, which requires multiple sets of primers to detect about 90% of human-infecting strains [3]. This method has significant equipment and expertise requirements, which are often not available outside of large institutions. Further, the expense of running multiple samples and the need for timely instrument accessibility limit the feasibility of applying RT-PCR as point-of-care applications or for preventing the rapid spread of an outbreak.
Other existing methods include immune electron microscopy (IEM) and enzyme immunoassays. IEM was the first method described for identifying NoVs and was used originally to classify viruses based on structural appearance. This method has limited sensitivity, and also requires expensive equipment and skilled expertise. Enzyme immunoassays, developed after the discovery of type-specific antibody epitopes on the NoV capsid, detect viral particles in human stool samples [4]. This method offers increased specificity and has led to the development of commercially available ELISA and lateral flow assays.
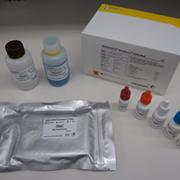
Currently, the only FDA-approved antigen detection assay is an ELISA called RIDASCREEN® (3rd Generation) produced by R-Biopharm, which uses an antibody cocktail with specificity for GI and GII NoVs [Fig. 1]. Due to limitations in sensitivity, this assay is only approved for use during outbreaks and takes several hours to produce results. Several companies, including R-Biopharm, have developed rapid diagnostic assays that use lateral flow technology and have also demonstrated strong specificity for NoV GI and GII strains. However, these have similar limitations with sensitivity and thus are only recommended for preliminary screening to be confirmed by RT-PCR, and are distributed primarily outside of the United States [5]. Overall, there is a clear need for improved diagnostic methods to detect norovirus rapidly with strong specificity, high sensitivity, and with minimal equipment and expertise requirements.
Novel diagnostic phage reagents
Recent studies in our laboratory have identified short, 12-mer peptide reagents with specific binding to the GI.1 NoV genotype [6]. The small size of these peptides displayed on phages offers the ability to access epitopes that may be buried in the capsid protein and not accessible to antibodies, and the potential for increased avidity through multiple linked peptide molecules. To identify peptides with specific binding to NoV, we used phage display technology to screen commercially available, large-scale libraries of randomized peptides that are fused to the gene III protein and expressed in five copies on one end of the phage. Rounds of biopanning were performed in which filamentous phage libraries were screened for phages displaying peptides that bind immobilized Norwalk (NV) GI.1 virus-like particles (VLPs). The phage libraries were added to VLPs and, after washing away non-binding phages, the phages displaying VLP-binding peptides were eluted with low pH [Fig. 2A]. Two to four subsequent rounds of biopanning using the resulting phage populations enriched for phages displaying peptides with the highest binding affinity for NV. DNA sequencing of individual phage clones recovered after multiple rounds of biopanning revealed three peptides, named NV-O-R5-3, NV-O-R5-6, and NV-N-R5-1, that occurred most commonly, and the phage clones displaying the peptides were further characterized for their NoV binding properties [6].
Phage-based ELISAs confirmed the binding specificity of phage-displayed peptides to NV VLPs. These affinity-binding assays used NV VLP captured by immobilized rabbit polyclonal anti-NV antibody in order to maintain the structural integrity of VLPs. Single phage clones were added to the captured VLPs and binding was detected using anti-M13 phage antibody that was conjugated to horseradish peroxidase to provide a signal for bound antibody [Fig. 2B]. Of the three peptide-displaying phage clones analysed, NV-N-R5-1 exhibited a dose-dependent response with decreasing NV VLP concentration and the highest sensitivity with a limit of detection at 1.56 ng NV VLP. Additional phage ELISAs indicated that NV-N-R5-1 binds to the P domain of the capsid protein, which extends the furthest out from the virus, and has comparable sensitivity for NV as existing antibodies used for diagnostics [6]. These results provide proof-of-concept and a strong lead reagent for developing novel phages displaying peptides as effective detection reagents for NoV. Further, the methods described establish a platform methodology for using phage display to identify antigen-specific binding reagents that may be applied to any pathogen with distinct surface epitopes.
Current status
To develop our lead phage-displayed peptide into a commercially viable tool, we are currently optimizing its binding affinity for other genogroups of NoV in order to broaden its diagnostic applications. Phage display technology provides a simple platform for constructing collections of new mutations in a lead peptide that can be used for additional rounds of biopanning to screen for variants with optimal affinity properties [Fig. 2C]. The three phage-displayed peptides discussed above share conserved amino acid sequence motifs that likely confer binding specificity for particular epitopes on the NV capsid protein. Directed evolution through mutagenesis of amino acids surrounding these consensus sequences can enable us to improve binding affinity to NV and alter binding specificities starting with the lead phage peptide, NV-N-R5-1. In particular, developing phage-displayed peptides with optimized binding affinity for the NoV GII.4 genotype, which accounts for >80% of NoV infections worldwide [1], and other GI and GII NoV genotypes will have the greatest relevance for diagnostic applications.
Future development of bacteriophage reagents
For decades, phages have been used to identify their target bacterial strains and species in order to diagnose the cause of infections by phage typing. More recent applications have begun to leverage synthetic biology and genomic engineering strategies to customize phage specificity and reporter signals to enable ‘near-real-time’ detection of a broader range of human pathogens [7]. Our recent work has established a methodology for the identification, characterization, and development of phage-based affinity reagents that may be applied to different pathogens and translated into diagnostic applications. The process outlined in Figure 2 demonstrates the progression from (A) identifying lead reagents against a target of interest, (B) characterizing binding affinity for the antigenic target, (C) optimizing leads through directed evolution or genomic engineering strategies, and finally (D) producing scalable quantities of reagent for commercial diagnostic applications. Zou and colleagues, for example, used a similar method to identify a phage-displayed peptide reagent with specific binding to transmittable gastroenteritis virus (TGEV) that also showed potential antiviral activity [8]. Several groups have also developed phage-based reagents to detect bacterial pathogens, such as Salmonella enterica and Escherichia coli [9, 10].
In summary, the use of phage-based reagents for microbial diagnostics offers many advantages in comparison to more commonly used detection reagents, such as antibodies. Phage display technology enables rapid identification and validation of candidate phage reagents with specificity for new or evolved pathogens through biopanning of commercial or custom made phage libraries (Fig. 2A, B). Phage manipulation through directed evolution facilitates development of reagents with optimized binding affinity and specificity to a target of interest (Fig. 2B). Finally, production of large quantities of phages is accomplished rapidly and inexpensively, as simple preparation methods can produce sufficient phage for hundreds of assays (Fig. 2D). As viral pathogens such as NoV continually evolve, the flexibility provided by phage-based reagents will be essential for developing next generation diagnostics for effective containment of outbreaks. A cocktail of phages, each of which binds to a specific target NoV genotype, may ultimately be the ideal strategy for producing an assay to detect the broadest possible range of NoVs without sacrificing specificity. Overall, phages have an enormous potential for use as detection reagents in clinical, agricultural, food, and environmental settings, and represent an underutilized resource for diagnostic development.
References
1. Donaldson EF, Lindesmith LC, Lobue AD, Baric RS. Norovirus pathogenesis: mechanisms of persistence and immune evasion in human populations. Immunological Reviews 2008; 225(1): 190–211.
2. Kroneman A, Vega E, Vennema H, Vinjé J, White P, Hansman G, Green K, Martella V, Katayama K, Koopmans M. Proposal for a unified norovirus nomenclature and genotyping. Archives of Virology 2013; doi:10.1007/s00705-013-1708-5.
3. Atmar RL, Estes MK. The epidemiologic and clinical importance of norovirus infection. Gastroenterology Clinics of North America 2006; 35(2): 275–290.
4. Parker TD, Kitamoto N, Tanaka T, Hutson AM, Estes, MK. Identification of Genogroup I and Genogroup II broadly reactive epitopes on the norovirus capsid. Journal of Virology 2005; 79(12): 7402–7409.
5. Ambert-Balay K, Pothier P. Evaluation of 4 immunochromatographic tests for rapid detection of norovirus in faecal samples. Journal of Clinical Virology 2013; 56(3): 194–198.
6. Rogers JD, Ajami NJ, Fryszczyn BG, Estes MK, Atmar RL, Palzkill TG. Identification and characterization of a peptide affinity reagent for detection of noroviruses in clinical samples. Journal of Clinical Microbiology 2013; 51(6): 1803–1808.
7. Lu TK, Bowers J, Koeris MS. Advancing bacteriophage-based microbial diagnostics with synthetic biology. Trends in Biotechnology 2013; 31(6): 325–327.
8. Zou H, Zarlenga DS, Sestak K, Suo S, Ren X. Transmissible gastroenteritis virus: Identification of M protein-binding peptide ligands with antiviral and diagnostic potential. Antiviral Research 99(3): 383–390.
9. Schofield DA, Sharp NJ, Westwater C. Phage-based platforms for the clinical detection of human bacterial pathogens. Bacteriophage 2012; 2(2): 105–283.
10. Galikowska E, Kunikowska D, Tokarska-Pietrzak E, Dziadziuszko H, Loś JM, Golec P, Węgrzyn G, Loś M. Specific detection of Salmonella enterica and Escherichia coli strains by using ELISA with bacteriophages as recognition agents. European Journal of Clinical microbiology & Infectious Diseases 2011; 30(9): 1067–1073.
The authors
Amy M. Hurwitz1 BS, Robert L. Atmar2,3 MD, Timothy G. Palzkill*2,4 PhD
1 Interdepartmental Graduate Program in Translational Biology and Molecular Medicine, Baylor College of Medicine, Houston, Texas, USA
2 Department of Molecular Virology and Microbiology, Baylor College of Medicine, Houston, Texas, USA
3 Department of Medicine, Baylor College of Medicine, Houston, Texas, USA
4 Department of Pharmacology, Baylor College of Medicine, Houston, Texas, USA
*Corresponding author
E-mail: timothyp@bcm.edu