Use of an LC-MS/MS 13-steroid serum panel in the diagnosis of adrenocortical carcinoma
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is increasingly becoming the method of choice in the clinical laboratory for the measurement of low molecular weight analytes. The major advantage that LC-MS/MS possesses relative to conventional laboratory techniques such as immunoassay is its higher specificity (and often sensitivity, although this is compound specific) and its ability to measure multiple compounds in a single run (multiplexing). LC-MS/MS thus provides the opportunity for more accurate and precise biochemical diagnosis and monitoring of human disease. One example of the increasing adoption of LC-MS/MS by clinical laboratories is the measurement of steroid hormones in various matrices (serum, saliva, urine).
Steroid metabolism
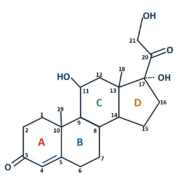
All steroids share a cyclopentanoperhydrophenanthrene nucleus, with individual species varying according to the presence of different functional groups attached to this four-ring structure, as well as by the oxidation state of the rings. Cortisol structure is given as an example in Figure 1. In humans, the major sites of steroid hormone production are the adrenal gland and the gonads. Steroids are synthesized from cholesterol via a series of enzyme-catalysed steps (Fig. 2), which are under tight regulation in healthy individuals by feedback mechanisms involving the hypothalamus and anterior pituitary. Steroids have a wide range of physiological functions which are summarized in Table 1.
Adrenocortical carcinoma – a diagnostic challenge
There are many endocrine disorders that result in the improper synthesis of steroids, and one of the rarest and most severe is adrenocortical carcinoma (ACC). ACC is a malignancy of the adrenal cortex with an annual incidence of 1 or 2 cases per million [1]. The majority of ACC cases are sporadic and occur in the fifth or sixth decade of life and more commonly in women; although ACC can be associated with several familial syndromes including Li-Fraumeni, Beckwith-Wiedemann, Lynch syndrome and multiple endocrine neoplasia type 1 [2]. Functional steroid hormone-producing tumours occur in around two-thirds of cases [3], presenting with varied signs and symptoms of steroid overproduction, most commonly Cushing’s syndrome (cortisol excess) and hyperandrogenism. ACC can progress rapidly in some patients, therefore it is vital that it is distinguished from benign adrenal adenomas, as ACC has a 5-year survival rate of <50% [2]. A surgical cure is only possible if the carcinoma is detected in its localized stage, otherwise the median survival period is <15 months [4].
The diagnosis of ACC is challenging as there is no single diagnostic tool that is able to distinguish ACC from other adrenal masses, including benign adenomas with glucocorticoid or mineralocorticoid excess, phaeochromocytoma and non-functioning adenomas. Imaging alone is insufficient for diagnosis, as although patients with ACC almost always present with tumours ≥4 cm, the presence of a large mass only has a clinical specificity of 61% [5]. Additionally, whereas up to two-thirds of tumours are functional, less than half of ACC cases present with clinical signs of steroid overproduction [3], with a further proportion presenting with other symptoms including abdominal pain. However, a significant proportion are discovered incidentally [2].
The European Network for the Study of Adrenal Tumours (ENSAT) currently recommends that the initial biochemical work-up for suspected ACC includes measurement of serum cortisol (both basal and assessment of suppression after dexamethasone), dehydroepiandrostenedione sulphate (DHEAS), androstenedione, testosterone, 17-hydroxyprogesterone, estradiol and aldosterone (if the patient is hypokalemic or hypertensive). An alternative approach is to measure steroid metabolites in urine using gas chromatography-mass spectrometry (GC-MS); increases in the excretion of metabolites of the steroid precursors 11-deoxycortisol, 17-hydroxypregnenolone and pregnenolone have been shown to provide particularly high diagnostic utility in ACC. Unfortunately, urine steroid profiling is not commonly available in clinical laboratories owing to lengthy sample preparation and complex result interpretation. Further, serum 11-deoxycortisol, 17-hydroxypregnenolone or pregnenolone measurements are rarely performed either because of lack of demand, or specificity of the available immunoassays which may be subject to significant levels of cross-reactivity.
As a result of these limitations, the use of LC-MS/MS is increasingly being adopted to provide more specific steroid hormone measurements. An approach we have taken in our laboratory is to develop and fully evaluate a multiplexed LC-MS/MS method panelling 13 steroids in serum [6] to include many of the steroid synthetic pathway intermediates currently not available for ACC work-up.
Use of a serum steroid panel
The steroids included in our serum panel are highlighted in Figure 2 and are as follows:
- androstenedione
- corticosterone
- cortisol
- cortisone
- 11-deoxycorticosterone
- 11-deoxycortisol
- 21-deoxycortisol
- DHEAS
- 17-hydroxypregnenolone
- 17-hydroxyprogesterone
- pregnenolone
- progesterone
- testosterone.
Samples are prepared for analysis by an initial protein precipitation step to remove steroids from their binding proteins, followed by liquid-liquid extraction in order to cleanly extract the steroids from remaining matrix components. Prepared extracts are then analysed by LC-MS/MS in which steroids are first resolved on a reverse phase C18 column by gradient elution followed by MS/MS detection using positive atmospheric pressure chemical ionization (APCI) operated in multiple reaction monitoring mode. Chromatographic separation of several isobaric (same mass to charge ratio) steroids is essential, as is the use of deuterated internal standards for all steroids in the method.
When we applied our method to adrenal tumour samples [6], we were able to show that between 4 and 7 steroids were elevated in all ACC cases in comparison to non-ACC adrenal tumours where a maximum of 1–2 steroids were abnormal. The cortisol precursor 11-deoxycortisol was most useful in the discrimination between ACC and non-ACC adrenal lesions, whereas other steroids markedly elevated in ACC included 17-hydroxypregnenolone and pregnenolone. Indeed, all steroids except testosterone in males and corticosterone and cortisone in both sexes were of use in discriminating ACC. This validates the use of a panelling approach when investigating adrenal masses.
Our findings compare well with urine steroid profiling studies. Although urine steroid profiling using 24-hour collections may offer greater clinical sensitivity compared to a single blood measurement owing to diurnal rhythms of steroid production, urine measurements rely on accurately timed collections that are often performed incorrectly and are inconvenient to the patient. Advantages of our LC-MS/MS serum panel compared to urine steroid profiling by GC-MS include a less labour intensive sample preparation, as well as less expertise required for the interpretation of complex profiles, as the serum method only targets selected steroids rather than the large number of their metabolites in urine.
Use of our LC-MS/MS serum steroid panel in ACC patients has further demonstrated the limitations of assessing serum steroids by immunoassay. We observed evidence of notable interference in ACC patients in the cortisol, progesterone, 17-hydroxyprogesterone and androstenedione immunoassays, inferred to be due to elevated concentrations of structurally related steroid precursors.
Future work
Currently, our 13-steroid serum panel has been used to study a relatively small number of ACC patients (because of the rarity of the disease), and clearly larger prospective studies are required to more fully determine the diagnostic utility of our panel in ACC. Further work is also required to clarify the effects of age, sex and diurnal variation on serum steroid panelling; nonetheless the most useful markers of ACC are markedly elevated above variation attributable to these biological factors. In addition to the complexity of interpreting biomarker panels, it is not only important to consider specific reference ranges, but to also consider the patterns in results which require an omics-based analysis approach to interpretation. The challenge surrounding this, as well as the requirement for clear presentation and reporting of results to clinicians requires close involvement of clinical colleagues for the development and introduction of such testing strategies.
The analysis of steroid panels by LC-MS/MS can also undoubtedly be used in other conditions including inborn errors of steroid metabolism such as congenital adrenal hyperplasia (CAH) and polycystic ovarian syndrome (PCOS).
Although we have demonstrated the advantages of our LC-MS/MS steroid panel compared to routine immunoassays, there are undoubtedly disadvantages of using LC-MS/MS. These include the initial cost of instrument purchase, the increased expertise required and often a more laborious sample preparation. Additionally, the specificity of mass spectrometry should not be readily assumed; careful selection of multiple reaction monitoring (MRM) transitions and chromatography conditions are essential to separate isobaric steroids and other interfering compounds. However, in the context of improving the biochemical tools available to us to aid the diagnosis of ACC, the advantages of LC-MS/MS far outweigh these limitations.
Summary
In summary, LC-MS/MS serum steroid panelling offers an additional tool for the challenge that is the diagnosis of ACC. Our method combines measurement of both common and rarely measured steroids in a single sample, which we have shown provides useful data to aid the discrimination of ACC from benign adrenal tumours. Use of LC-MS/MS gives several advantages over the immunoassay and GC-MS-based methods currently used to assess steroid overproduction, but further work is required to demonstrate the full potential of its use in the diagnosis of ACC.
References
1. Fassnacht M, Kroiss M, Allolio B. Update in adrenocortical carcinoma. J Clin Endocrinol Metab 2013; 98: 4551–4564.
2. Else T, Kim AC, Sabolch A, Ramond VM, Kandathil A, Caoili EM, Jolly S, Miller BS, Giordano TJ, Hammer GD. Adrenocortical carcinoma. Endocr Rev 2014; 35: 282–326.
3. Arlt W, Biehl M, Taylor AE, Hahner S, Libé R, Hughes BA, Schneider P, Smith DJ, Stiekema H, et al. Urine steroid metabolomics as a biomarker tool for detecting malignancy in adrenal tumours. J Clin Endocrinol Metab 2011; 96: 3775–3784.
4. Fassnacht M, Terzolo M, Allolio B, Baudin E, Haak H, Berruti A, Welin S, Schade-Brittinger C, Lacroix A, et al. Combination chemotherapy in advanced adrenocortical carcinoma. N Engl J Med 2012;366:2189–2197.
5. Hamrahian AH, Ioachimescu AG, Remer EM, Motta-Ramirez G, Bogabathina H, Levin HS, Reddy S, Gill IS, Siperstein A, Bravo EL. Clinical utility of noncontrast computed tomography attenuation value (Hounsfield units) to differentiate adrenal adenomas/hyperplasias from nonadenomas: Cleveland Clinical experience. J Clin Endocrinol Metab 2005; 90: 871–877.
6. Taylor DR, Ghataore L, Couchman L, Vincent RP, Whitelaw B, Lewis D, Diaz-Cano S, Galata G, Schulte KM, et al. A 13-steroid serum panel based on LC-MS/MS: use in detection of adrenocortical carcinoma. Clin Chem 2017; 63: 1836–1846.
The authors
Victoria Treasure* MSc and Dr David Taylor PhD
Department of Clinical Biochemistry
(Viapath), King’s College Hospital NHS Foundation Trust, London, UK
*Corresponding author
E-mail: Victoria.treasure@nhs.net