Flow cytometry and immunophenotyping for chronic lymphoproliferative disorders
Modern hematology emphasizes a multiparametric diagnostic approach and the basic parameters, beside history of the disease and clinical examination, are morphological, immunophenotypic and genetic evaluation. Flow cytometry plays an important role in diagnosis of a large group of hematological diseases. This article reviews the basic principles of flow cytometry and its use in hematology diagnosis, with emphasis on chronic lymphoproliferations.
by Dr Nataša Lazić
Introduction
In modern diagnostics, flow cytometry has an important place as one of the basic and irreplaceable tools for diagnosis, classification, monitoring and prediction of malignant hematological disease [1]. The extreme complexity of these diseases, on one hand, and the availability of the different therapeutic protocols for the different types of these diseases on the other, makes accurate and precise diagnosis imperative. Contributing to this is the fact that the World Health Organization (WHO), in the Classification of Tumours of Hemopoietic and Lymphoid Tissues, suggests a multiparametric approach in diagnosing these diseases; basic parameters required are morphological, immunophenotypic and genetic analysis for each entity of the disease, in addition to a detailed history of the disease and clinical examination [2, 3]. The clinical picture and cell morphology, as a well-known and traditionally-used means of examination, are insufficient in many cases; quite often, because of a similar clinical presentation and cell morphology, it is not possible to draw a diagnostic conclusion based on these findings or a wrong diagnosis may be reached in some cases.
Coulter’s principle of measuring the change in the electrical impedance of the individual cells flowing through the measuring cell, in the late 1940s, was the basis for construction of the first hematologic counter and later for the flow cytometer. Later inventions added new detection capabilities, such as light scatter and fluorescence detection. Fluorescent activated cell sorting (FACS) was invented in the late 1960s by Herzenberg, Bonner, Sweet and Hullet. Introduced as a commercial machine in the early 1970s, this is the class of instruments now commonly referred to as flow cytometer [4]. The invention of monoclonal antibodies by Milstein and colleagues in 1977 opened new perspective for flow cytometry. Further developments, especially in electronics, led to modern cytometers with multiple lasers, detectors, better performance characteristics, and the ability to measure larger amounts of data.
Flow cytometry principles
Flow cytometry is a powerful technology that simultaneously measures many aspects of single particles, usually cells. Any suspended particle or cell from 0.2–150 μm is suitable for analysis. However, it can also measure soluble molecules if trapped onto a particulate surface and bound by fluorochromes. Virtually any component or function of a cell can be measured if the fluorescent probe can be made to detect it.
Sample preparation should provide a homogeneous suspension of cells with monoclonal antibodies conjugated with fluorochromes of a different emission spectrum. Depending on the sample, it most often includes incubation, erythrocyte lysis, centrifugation, washing and fixation.
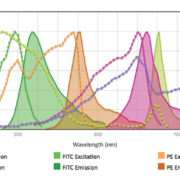
The cytometer needs to be adjusted to have the appropriate performance characteristics (linearity, sensitivity, CV, electronic and optical background noise, fluorescence detector efficiency, etc). This is achieved by adjusting voltages on the detectors and by spectral overlap compensation (Fig. 1).
The three main systems of flow cytometer are fluidics, optics and electronics (Fig. 2). Parameters measured include forward scatter (FSC) corresponding to cell size, side scatter (SSC) depending on internal complexity and fluorescence intensity for different fluorochromes.
Becoming more available in clinical laboratories, a wide range of clinical applications of flow cytometry are constantly expanding and the most common among them are in, for example, lymphoma and leukemia diagnosis, stem cell enumeration for transplantation, estimation of minimal residual disease, paroxysmal nocturnal hemoglobinuria diagnosis, immunodeficiencies, HIV infection.
Flow cytometry in hematology
Flow cytometric immunophenotyping enables examination of the phenotype of the separate cells in the suspension and summarizing of the results, which gives data about the presence or absence of antigen expression as well as the expression intensity [5]. Hence, an immunophenotypic pattern is obtained on the cell population of interest for the examined disease. Meanwhile, there are no separate antigens specific for the particular disease. Instead, their mutual relation is observed and analysed, which makes the analysis of the flow cytometry results very demanding and complex, but usually very useful and precise owing to the huge amount of data that can be collected from the cells [6]. Therefore, flow cytometry helps with determining the cell line, the degree of cell maturity, abnormal patterns of expression and provides a detailed immunophenotype of the pathological cell population [7]. From information on all the aforementioned factors, a diagnostic conclusion is drawn if there is a phenotype characteristic for some disease. In the case of an atypical phenotype, the disease is assigned to the appropriate group and additional tests should be done to gain a precise diagnosis (such as immunohistochemical, FISH, molecular tests).
CD markers (clusters of differentiation) are blood cell antigens that enable their characterization. CD nomenclature was developed and reviewed by HLDA (Human Leukocyte Differentiation Antigen) workshops started in 1982. There were 10 such workshops and the nomenclature now encompasses about 400 CD markers. Monoclonal antibodies against those antigens are used for immunophenotype characterization.
The antibody panel for the analysis of the sample to be tested by flow cytometry depends, to a large extent, on the available information of other findings made for that patient. According to the Bethesda Group recommendations from 2006, which were aimed at regulating a more systematic approach in this field (and are still valid today), before sending a sample to flow cytometry, a detailed history of the disease, clinical examination, microscopic examination of cell morphology, and other laboratory tests should be carried out, and based on this, diagnosis or differential diagnosis determined. In this way significant rationalization and cost reduction can be achieved [8].
Immunophenotype characterization for chronic lymphoproliferative disorders
For both of the two major groups of malignant hematologic diseases, those derived from mature and from immature cells, flow cytometry is of a great importance. Neoplasms of mature lymphoid cells, according to the WHO Classification, include chronic lymphoid leukemia and non-Hodgkin’s lymphoma. Their basic characteristic is that they have an immunophenotype similar to mature lymphoid cells and, accordingly, they show an absence of immaturity indicators (CD34, TdT). According to the origin, in relation to the cell line, they can be divided into T, B and NK neoplasms. [7]
Mature B-cell lymphoproliferations make up most of the malignant blood diseases: 90 % of the total lymphoid malignancies, according to WHO data. They present 4 % of the newly discovered carcinomas per year. As already known, the malignant cell derived from B-cell lineage in most cases imitates the normal B-cells stopped at a certain maturity level. The classification of this disease group mostly relies on this fact. The most common in this group are chronic lymphocytic leukemia (CLL), hairy cell leukemia (HCL), follicular lymphoma, splenic marginal zone lymphoma, mantle cell lymphoma (MCL), plasma cell leukemia [12]. Immunophenotype characterization in the diagnosis of B-cell chronic lymphoproliferative diseases is an irreplaceable method and, together with morphology, it presents the essential search that should be undertaken in the diagnosis of these diseases[2, 9]. Based on the finding of the immunophenotype characterization it is possible to discover aberrant expression patterns and establish the phenotypic characteristics related to particular diseases. The application of a scoring system as an additional tool is the result of a need for some standardization and quantification in the diagnosis of B-cell chronic lymphoproliferative diseases. In order to increase the precision of the scoring system, different studies with different CD markers are taken [10–12]. The most common scoring system of 5 points includes CD5, CD23, FMC7, CD79b and surface immunoglobulin chains with an accuracy of 96.6 % if a three-point cut-off is used [10].
In most cases of CLL, cell morphology is characteristic and typical for this disease. However, in a number of cases, flow cytometry has a huge and decisive significance for diagnosis (Fig. 3) [13]. CLL and MCL share many morphological and immunophenotypic features [14]. As a result of their partial overlap, a differential diagnosis of MCL is most considered when making a diagnosis of CLL. Because of the different therapeutic approach and prognoses of the diseases, their diagnostic differentiation is very important. For that purpose cyclin D1 testing is recommended [15, 16]. Unlike the other chronic lymphoproliferations, HCL cells do not match any stage of the normal lymphoid cells development. Morphologically typical HCL cells have fine, hair-like, cytoplasmic projections, which are sometimes difficult to find in the peripheral blood smear. Because of this and a very specific immunophenotype, flow cytometry is essential for HCL diagnosis [14, 17].
Advantages
The possibility of combining more antibodies in the same tube and analysing their interactions on the population of interest for the given disease is the greatest advantage of multiparametric flow cytometry, which involves simultaneously collecting and analysing a large amount of data from cells or particles.
Considerations
Comprehensive analysis involves considering possible causes of false-positive or false-negative results, thus avoiding an incomplete or incorrect interpretation of flow cytometry data (Fig. 4).
Other difficulties, such as non-standardized methods, particularly the issue of regulation in cytometry, different antibody panels, cut-off values, analysis subjectivity – recommended visual approach, result analysis complexity, report form, etc., are the subject of work by various associations dealing with cytometry in order to achieve harmonization in this area [13].
References
1. Paiva A, Alves GVA, Sales VSF, Silva ASJ, Silva DGKC, Alves E, Bahia F, Freitas RV, De Oliveira Paiva HD, Cavalcanti GB, Jr. Utility of flow cytometry immunophenotyping and hematological profile in chronic lymphoproliferative disorders. Blood 2017; 130: 5326 [poster abstract].
2. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman J (eds). WHO classification of tumors of haematopoietic and lymphoid tissues. IARC 2008; Chapters 1, 8, 10. ISBN 978-9283224310.
3. Boyd SD, Natkunam Y, Allen JR, Warnke R. Selective immunophenotyping for diagnosis of B-cell neoplasms: immunohistochemistry and flow cytometry strategies and results. Appl Immunohistochem Mol Morphol 2013; 21: 116–131.
4. Herzenberg LA, Parks D, Sahaf B, Perez O, Roederer M, Herzenberg LA. The history and future of the fluorescence activated cell sorter and flow cytometry: a view from Stanford. Clin Chem 2002; 48: 1819–1827.
5. Braylan RC. Impact of flow cytometry on the diagnosis and characterization of lymphomas, chronic lymphoproliferative disorders and plasma cell neoplasias. Cytometry A 2004; 58: 57–61.
6. Brown M, Wittwer C. Flow cytometry: principles and clinical applications in hematology. Clin Chem 2000; 4: 1221–1229.
7. Craig FE, Foon FA. Flow cytometric immunophenotyping for hematologic neoplasms. Blood 2008; 111: 3941–3967.
8. Oberley MJ, Fitzgerald S, Yang DT, Morgan A, Johnson J, Leith C. Value-based flow testing of chronic lymphoproliferative disorders: a quality improvement project to develop an algorithm to streamline testing and reduce costs. Am J Clin Pathol 2014; 142: 411–418.
9. D’Arena G, Keating MJ, Carotenuto M. Chronic lymphoproliferative disorders: an integrated point of view for the differential diagnosis. Leuk Lymphoma 2000; 36: 225–237.
10. Matutes E, Wotherspoon A, Catovsky D. Differential diagnosis in chronic lymphocytic leukemia. Best Pract Res Clin Haematol 2007; 20: 367–384.
11. Matutes E, Owusu-Ankomah K, Morilla R, Garcia Marco J, Houlihan A, Que TH, Catovsky D. The immunological profile of B cell disorders and proposal of a scoring system for the diagnosis of CLL. Leukemia 1994; 8: 1640–1645.
12. Moreau EJ, Matutes E, A’Hern RP, Morilla AM, Morilla RM, Owusu-Ankomah KA, Seon BK, Catovsky D. Improvement of the chronic lymphocytic leukemia scoring system with the monoclonal antibody SN8 (CD79b). Am J Clin Pathol 1997; 108: 378–382.
13. Rawstron AC, at al. Reproducible diagnosis of chronic lymphocytic leukemia by flow cytometry: an European Research Initiative on CLL (ERIC) & European Society for Clinical Cell Analysis (ESCCA) Harmonisation project. Cytometry B Clin Cytom 2018; 9: 121–128.
14. Asaad NY, Abd El-Wahed MM, Dawoud MM. Diagnosis and prognosis of B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma (B-CLL/SLL) and Mantle cell lymphoma (MCL). J Egypt Natl Canc Inst 2005; 17: 279–290.
15. Matutes E, Polliack A. Morphological and immunophenotypic features of chronic lymphocytic leukemia. Rev Clin Exp Hematol 2000; 4: 22–47.
16. Vose JM. Mantle cell lymphoma; update on diagnosis, risk stratification and clinical management. Am J Hematol 2015; 90: 739–745.
17. Bacal NS, Mantovani E, Grossl S, Nozawa ST, Kanayama RH, Brito ACM, Albers CEM, de Campos Guerra JC, Mangueira CLP. Flow cytometry: immunophenotyping in 48 hairy cell leukemia cases and relevance of fluorescence intensity in CDs expression for diagnosis. Einstein 2007; 5: 123–128.
The authors
Nataša Lazić MD
Institute for Clinical Laboratory Diagnostics, University Clinical Centre of the Republika Srpska, Republika Srpska, Bosnia and Herzegovina
*Corresponding author
E-mail: natasa.lazic.bl@gmail.com