Chromogranin A as a biomarker for the detection of neuroendocrine tumours
Neuroendocrine tumours (NETs) are a heterogeneous group of tumours that vary depending on their anatomical sites, functionality and hormones produced. They are often silent clinically, and diagnosis is usually delayed. Chromogranin A (CgA) is the best-known general biomarker which is used for the diagnosis and management of NETs. It can be measured in serum or plasma using different analytical methods that include RIA, IRMA or ELISA. Raised circulating CgA is considered to be a relatively sensitive marker for the diagnosis of NET. As the test is rather non-specific, the diagnostic yield can be improved if other non-NET related conditions with raised CgA including renal failure, cardiac, hepatic and inflammatory diseases and use of proton pump inhibitor (PPI) are excluded.
by Dr Elham AlRisi and Prof. Waad-Allah S. Mula-Abed
Introduction
Neuroendocrine tumours (NETs) are a group of tumours that are usually derived from the cells of the nervous and endocrine systems. The tumours are characterized by being rare, heterogeneous and may affect different tissues and organs with neuroendocrine elements including the gastroenteropancreatic system, lungs, thyroid, parathyroid, pituitary, sympathoadrenals, and other tissues [1]. The NETs are distinctive in that their structural components of cells have the ability to synthesize, store, and secret bioactive amines and peptide hormones, a phenomenon termed ‘amine precursor uptake and decarboxylation’ (APUD) [2]. Although NETs may be considered rare, there is, however, increasing interest in their diagnosis, reported incidence and increased survival duration over time, suggesting that NETs are more prevalent than were previously reported.
The US Surveillance, Epidemiology, and End Results (SEER) Program registries in their search from 1973 to 2004, identified 35 618 patients with NETs with a significant increase in the reported annual age-adjusted incidence of NETs from 1973 (1.09/100 000) to 2004 (5.25/100 000). Using the SEER registry data, the estimated 29-year limited-duration prevalence of NETs in January 2004, was found to be 9263 and the estimated 29-year limited-duration prevalence in the United States on that date was 103 312 cases (35/100 000) [3]. The clinical presentations in patients with NETs vary according to the site where the tumour develops, which can be anywhere in the body and can range from a silent tumour, to one that is associated with an overproduction of the hormone/peptide (with their pathophysiological and clinical sequels) known to be produced by that tissue, or to a metastatic tumour. The growing interest in NETs in recent years is attributed to the increasing medical awareness, availability of laboratory markers for the detection of NETs particularly the chromogranins and the wide use of radiological imaging that have increased the diagnostic yields of these tumours.
Physiology of the granin family including chromogranin A
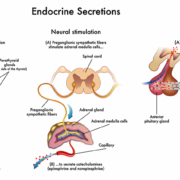
The secretory granules of the neuroendocrine and endocrine cells contain a family of highly acidic proteins, the granins. The most abundant forms of granins are chromogranin A (CgA), chromogranin B (CgB), secretogranin II (SgII), whereas granins the other forms that include SgIII, VGF, 7B2, and proSAAS are much less distributed in these granules. The granins are involved in the granulogenesis of the secretory granule biogenesis, with some being processed to form numerous peptides that have different physiological activities. CgA, the most studied chromogranin, was first isolated from the chromaffin cells of the adrenal medulla. It is a single polypeptide chain of 439 amino acids and 10 dibasic cleavage sites; the CgA gene is localized on chromosome 14q32 [4, 5].
Chromogranins contribute intracellularly to the overall vesicle biogenesis and facilitate the processing and regulation of other secretory proteins. Processing of chromogranins gives rise to multiple bioactive peptides that include the vasodilator vasostatin (human CgA 1–76), catecholamine release inhibitor catestatin (human CgA 352–372) and dysglycemic peptide pancreastatin (human CgA 250–301) [6]. Pancreastatin regulates glucose metabolism in cells and certain organs by inhibiting glucose-mediated insulin release from pancreatic islet cells, and inhibiting glucose uptake by adipocytes and hepatocytes. Other contributing functions of CgA include its involvement in regulating endothelial barrier, tumour angiogenesis, anti-apoptosis, and vascular structure and permeability [7].
Laboratory methods for the measurement of chromogranin A
There are different approaches for the determination of circulating CgA. The currently available methods include radioimmunoassay (RIA), immunoradiometric assay (IRMA) and enzyme-linked immunosorbent assay (ELISA). The introduction of commercially available ELISA kits for CgA assay (with their advantages of having long shelf life, technical ease, safety of use, and reported reasonable validity) has greatly improved the measurement of CgA in the diagnosis and clinical management of patients with of NETS. Currently there is increasing availability of these kits for measuring CgA in many hospital laboratories.
CgA can be measured using plasma or serum specimens. Although plasma CgA has been reported in a few studies to be higher than in serum, the difference may not affect clinical interpretation, particularly if there is consistent use of a single specimen type [6]. Different results might be reported by the different techniques, which might affect the validity indicators using these techniques. There are no universal standards for the techniques used and no universally accepted technique. There are reports that favour RIA over other methods; however, the practical advantages of ELISA techniques, especially the long shelf life, might make them attractive methods for use by many laboratories and might explain their widespread use in today’s practice [8]. Nevertheless, the selection of the analytical method to be used depends on the technical feasibility and convenience in the laboratory.
Chromogranin A and neuroendocrine tumours
CgA and its fragments are usually present in the circulation in equimolar concentration with the secretory activity of the secreting neuroendocrine tissue of both normal subjects and patients with different NETs; hence, CgA concentration in the circulation can be measured to provide information on the diagnosis, prognosis and monitoring of patients with these tumours, if other non-NET related physiological, pathological and pharmacological causes are excluded.
CgA is usually secreted by a variety of NETs, which include: carcinoids, pheochromocytoma, paraganglioma, medullary carcinoma of thyroid, parathyroid adenomas, pulmonary NETs including small cell lung cancer, gastroenteropancreatic (GEP-NETs) including functioning and nonfunctioning pancreatic islet cell tumours, some pituitary adenomas and other APUD tumours. The highest CgA values are observed in small intestine NETs and GEP-NETs associated with MEN1. Moderate-to-high CgA values are noted in pancreatic NETs, Zollinger-Ellison syndrome and gastrinomas. CgA is more frequently elevated in well-differentiated tumours compared to poorly differentiated NETs [9]. Different clinical validity indicators for CgA have been reported by different workers in the different patient cohorts. Yang et al. through their search of 13 studies that included 1260 patients with NETs and 967 healthy controls, reported an overall sensitivity, specificity and diagnostic odds ratio (DOR) of 0.73, 0.95 and 56.3, respectively, while the summary positive likelihood ratio (PLR) and negative likelihood ratio (NLR) were 14.56 and 0.26, respectively [10]. In addition, the area under the curve (AUC) of the circulating CgA in the diagnosis of NETs was 0.896. The pooled sensitivity and specificity values of CgA were 0.73 and 0.95, respectively, whereas the pooled PLR and NLR values were 14.56 and 0.26, respectively for the diagnosis of NETs. All these data suggested a higher diagnostic accuracy of CgA for the diagnosis of NETs. Among the included studies, three different assays were used to measure the circulating CgA, the sensitivity was both 0.74 by ELISA and RIA assays, and 0.69 by IRMA assay. The specificity was 0.93, 0.95 and 1.00 for ELISA, RIA and IRMA assays, respectively.
CgA values also have a prognostic role, as their high levels correlate with poor prognosis and short survival in certain NETS [11]. This relationship is usually limited in patients with gastrinomas, who have high CgA values despite the small primary tumour size and absence of metastases, possibly due to CgA secretion from G cells. Also, CgA values reflect the tumour burden, and monitoring the disease by CgA usually helps in detecting tumour recurrence or progression following treatment by surgery or radiotherapy. In patients with midgut NET, serum CgA level was the first marker to reflect tumour recurrence compared with urinary 5HIAA and radiological measurements [12]. Also, in pheochromocytoma, especially when large and lacking the proper hormonal characterization, CgA may be the only laboratory guide in the diagnosis and management of patients with such tumours [13].
Pitfalls in the interpretation of chromogranin A values
Although CgA is a useful general marker for the diagnosis and management of NETs, its universal secretion by almost all neuroendocrine cells makes its use confounded by its co-elevation in a variety of non-NET conditions including non-NET malignancies [14–16]. Hence, interpretation of CgA results must be done in the context of the overall confounding factors, whether physiological, pharmacological or pathological. Such conditions include the use of proton pump inhibitors (PPIs) or H2-receptor blockers, chronic atrophic gastritis, impaired renal function, cardiac failure, hepatic insufficiency, inflammatory bowel disease, benign prostatic hypertrophy or malignancy, rheumatoid arthritis, untreated essential hypertension, and some non-NET neoplasms. The pattern of elevation in serum CgA in certain non-NET conditions has been suggested recently to be utilized as a biomarker and prognostic marker in the stratification of some chronic diseases. This is particularly the case for heart failure where CgA might have a role in identifying those at higher risk of short- or long-term mortality [17]. The role of CgA in diabetes is not clear. However, CgA and its cleavage fragments, including WE-14, might play a part in the pathogenesis of type 1 diabetes mellitus, possibly as a T-cell autoantigen in pancreatic β-cell destruction [18]. Therefore, CgA might have a potential use as a biomarker in the future [18].
Conclusion
Chromogranin A is a secretory protein of neuroendocrine origin that is usually present with its fragments in the circulation as a result of the secretory activity of the secreting neuroendocrine cells of both normal subjects and patients with different NETs. It is the best-known general biomarker which is increasingly used for the diagnosis and management of NETs. It can be measured in plasma or serum using different analytical methods that include RIA, IRMA or ELISA. Raised circulating CgA is considered to be a relatively sensitive marker for the diagnosis of NET particularly if there is clinical suspicion and other work-up investigations that are in plan. Its measurement is also of value in monitoring the progress of treatment and prognosis of the disease. The diagnostic yield is improved if other non-NET related diseases or conditions are considered and excluded prior to the interpretation of CgA values. These conditions include the use of PPIs or H2-receptor blockers, chronic atrophic gastritis, impaired renal, cardiac, or hepatic insufficiency, inflammatory bowel disease, rheumatoid arthritis, and some non-NET neoplasms.
References
1. Kaltsas GA, Besser GM, Grossman AB. The diagnosis and medical management of advanced neuroendocrine tumors. Endocr Rev. 2004; 25(3): 458–511.
2. Pearse AG. Common cytochemical and ultrastructural characteristics of cells producing polypeptide hormones (the APUD series) and their relevance to thyroid and ultimobranchial C cells and calcitonin. Proc R Soc Lond B Biol Sci. 1968; 170(1018): 71–80.
3. Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008; 26(18): 3063–3072.
4. Banks P, Helle K. The release of protein from the stimulated adrenal medulla. Biochem J 1965; 97(3): 40C–41C.
5. Bartolomucci A, Possenti R, Mahata SK, Fischer-Colbrie R, Loh YP, Salton SR. The extended granin family: structure, function, and biomedical implications. Endocr Rev. 2011; 32(6): 755–797.
6. Bech PR, Martin NM, Ramachandran R, Bloom SR. The biochemical utility of chromogranin A, chromogranin B and cocaine- and amphetamine-regulated transcript for neuroendocrine neoplasia. Ann Clin Biochem. 2014; 51(1): 8–21.
7. Taupenot L, Harper KL, O’Connor DT. The chromogranin-secretogranin family. N Engl J Med. 2003; 348(12): 1134–1149.
8. Stridsberg M, Eriksson B, Oberg K, Janson ET. A comparison between three commercial kits for chromogranin a measurements. J Endocrinol. 2003; 177(2): 337–341.
9. Modlin IM, Gustafsson BI, Moss SF, Pavel M, Tsolakis AV, Kidd M. Chromogranin A- biological function and clinical utility in neuro endocrine tumor disease. Ann Surg Oncol. 2010; 17(9): 2427–2443.
10. Yang X, Yang Y, Li Z, Cheng C, Yang T, Wang C, Liu L, Liu S. Diagnostic value of circulating chromogranin a for neuroendocrine tumors: a systematic review and meta-analysis. PLoS One 2015; 10(4): e0124884.
11. Ekeblad S, Skogseid B, Dunder K, Oberg K, Eriksson B. Prognostic factors and survival in 324 patients with pancreatic endocrine tumours treated at a single institution. Clin Cancer Res. 2008; 14(23): 7789–7803.
12. Welin S, Strisberg M, Cunningham J, Granberg D, Skogseid B, Oberg K, Eriksson B, Janson ET. Elevated plasma chromogranin A is the first indication of recurrence in radically operated midgut carcinoid tumors. Neuroendocrinology 2009; 89(3): 302–307.
13. Mula-Abed WA, Ahmed R, Ramadhan FA, Al-Kindi MK, Al-Busaidi NB, Al-Muslahi HN, Al-Lamki MA. A rare case of adrenal pheochromocytoma with unusual clinical and biochemical presentation: A case report and literature review. Oman Med J. 2015; 30(5): 382–390.
14. Gut P, Czarnywojtek A, Fischbach J, Bączyk M, Ziemnicka K, Wrotkowska E, Gryczyńska M, Ruchała M. Chromogranin A – unspecific neuroendocrine marker. Clinical utility and potential diagnostic pitfalls. Arch Med Sci. 2016; 12(1): 1–9.
15. Glinicki P, Jeske W. Chromogranin A (CgA) – the influence of various factors in vivo and in vitro, and existing disorders on its concentration in blood. Endokrynol Pol. 2011; 62(Suppl 1): 25–28 (in Polish).
16. Capellino S, Lowin T, Angele P, Falk W, Grifka J, Straub RH. Increased chromogranin A levels indicate sympathetic hyperactivity in patients with rheumatoid arthritis and systemic lupus erythematosus. J Rheumatol. 2008; 35(1): 91–99.
17. Goetze JP, Hilsted LM, Rehfeld JF, Alehagen U. Plasma chromogranin A is a marker of death in elderly patients presenting with symptoms of heart failure. Endocr Connect. 2014; 3(1): 47–56.
18. Stadinski BD, Delong T, Reisdorph N, Reisdorph R, Powell RL, Armstrong M, Piganelli JD, Barbour G, Bradley B, Crawford F, Marrack P, Mahata SK, Kappler JW, Haskins K. Chromogranin A is an autoantigen in type 1 diabetes. Nat Immunol. 2010; 11(3): 225–231.
The authors
Elham AlRisi MD; Waad-Allah S. Mula-Abed* MBChB MSc FRCPath
Directorate of Laboratory Medicine and Pathology, Royal Hospital, Muscat, Oman
*Corresponding author
E-mail: drsharef@live.com