The use of point-of-care ketone meters to diagnose and monitor diabetic ketoacidosis in pediatric patients
Children presenting with diabetic ketoacidosis (DKA) require prompt assessment and treatment initiation to prevent serious complications. The use of point-of-care (POC) analysers to assess blood ketones is beginning to replace the traditional analysis of urine ketones, but some questions remain as to their optimal utilization.
by Dr A.M. Ferguson, Dr J. Michael, Prof. S. DeLurgio and Dr M. Clements
Introduction
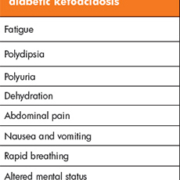
Diabetic ketoacidosis (DKA) is an acute complication of uncontrolled diabetes mellitus resulting from insulin deficiency. It is biochemically defined as hyperglycemia (blood glucose >200 mg/dL) with metabolic acidosis (venous pH <7.3 or bicarbonate <15 mmol/L), ketonemia, and ketonuria [1]. The clinical picture of the patient can include fatigue, polydipsia, polyuria, dehydration, abdominal pain, vomiting and altered mental status (Box 1). DKA can occur in known diabetics and can be the presenting symptom prior to diagnosis. Children who are on insulin pump therapy, who have unstable family situations, or have limited access to healthcare are at an increased risk of DKA [1], and DKA is the most common cause of diabetes-related mortality in children.
Assessing urine ketones has been part of the standard practice when assessing if a patient has DKA, but this has multiple issues. There are three types of ketones: acetoacetate, acetone, and β-hydroxybutyrate (BHB). BHB is the predominant ketone produced during DKA and can be present at up to 10 times the amount of acetoacetate. The urine dipsticks that are commonly used to assess ketonuria utilize a nitroprusside reagent that reacts with acetoacetate and acetone but not at all with BHB. This is problematic because the major ketone produced in DKA is not detected, which can lead to false negative urine ketone testing. Additionally, as ketosis resolves, BHB is converted to acetoacetate, increasing urine ketones during the recovery phase, potentially leading the clinician to believe that the ketosis is worsening instead of resolving. An added obstacle is the difficulty of getting a urine specimen from a young child, especially one in nappies. Measuring serum ketones, specifically BHB, is a solution to both of these issues.
Clinical measurement of serum ketones
As the methodology for measuring serum BHB became more automated, the test moved from being used only on a research basis to being available for clinical use. Initial studies were done to see how serum BHB functioned for the diagnosis of DKA. A large retrospective study looking at simultaneous measurements of BHB and bicarbonate found that BHB levels of ≥3 and ≥3.8 mmol/L in children and adults, respectively, could be used to diagnose DKA and provides a more specific assessment of DKA than bicarbonate alone [2].
When assessing patients for DKA, it is critical to make the diagnosis as quickly as possible to initiate treatment and prevent the patient from decompensating further. The commercial availability of point-of-care (POC) meters to assess serum ketones allows the patient to be tested immediately on presentation at the bedside. There have been multiple studies performed in adults showing that use of POC BHB meters in the emergency room can aid in diagnosis and treatment of DKA. Arora et al. compared POC BHB and urine ketone dipstick results in 54 patients with DKA presenting to the emergency department [3]. They found that both methods were equally sensitive for detecting DKA at 98.1%, but that BHB with a cut-off of ≥1.5 mmol/L is more specific for DKA compared to urine dipsticks (78.6 vs 35.1%) and could cut down on unnecessary DKA work ups in hyperglycemic patients. Another study found that a BHB value of 3.5 mmol/L yielded 100% sensitivity and specificity for the diagnosis of DKA [4].
Use of POC testing in pediatrics
Fewer studies have been done in pediatric patients. One such study by Ham et al. determined that using a POC meter in the hospital setting could aid in monitoring the resolution of DKA in pediatric patients [5]. The BHB values from the POC meter correlated with BHB values from the laboratory for most of the meter’s measurement range. Use of the meter had both a strong positive predictive value (PPV, 0.85) as well as negative predictive value (NPV, 1.0) for indicating the presence or absence of DKA at a meter value of 1.5 mmol/L [5]. Noyes et al. used POC ketone testing to identify the endpoint of an integrated care pathway when treating DKA in children [6]. They compared their current treatment endpoint of pH >7.3 and no presence of urine ketones with an endpoint defined by pH >7.3 and two successive POC ketone measurements of <1 mmol/L. The study measured time of treatment in 35 patient episodes in children ranging in age from 1–14 years. The time to completion of treatment using POC ketone measurement was 17 hours, compared to 28 hours using measurement of urine ketones to end treatment [6] . They found that occasionally a value below 1 mmol/L would be followed by a value above 1 mmol/L, but this never occurred after two subsequent values under 1 mmol/L, leading them to recommend waiting for the two successive low values before ending treatment. In addition to allowing an earlier treatment endpoint, this approach enables less time to be spent in the ICU, with decreased cost associated with treatment. Using a POC ketone meter can also result in fewer tests being ordered overall. Rewers and colleagues asked whether monitoring serum BHB values at the bedside could result in a decrease in laboratory testing in pediatric patients [7]. Their results indicated that the real-time changes observed in POC serum BHB values correlated strongly with changes in pH, bicarbonate, and pCO2 and also had good correlation with the laboratory BHB method. While initial measurement of pH, bicarbonate and pCO2 is encouraged, following up the patient with POC BHB can replace serial laboratory measurements of those analytes and decrease the amount of laboratory testing [7]. Similarly, a separate study showed that use of a POC BHB meter at home decreased diabetes-related hospital visits and hospitalizations of pediatric diabetics when compared to urine ketone testing by allowing earlier identification of ketosis and initiation of treatment [8].
Most of the studies mentioned are close to 10 years old, but measuring serum BHB to diagnose DKA or monitor its resolution has not become standard practice. A recent review of the standard treatment guidelines for DKA in children and adolescents raises the question of whether blood ketones should be evaluated during management of DKA [9]. The authors recommend using serum BHB measurement, either from the laboratory or at the point of care, to both diagnose DKA and monitor treatment. Despite the inaccuracies of POC meters seen at high BHB values [5–7], use of a diagnostic cut-off of >3 mmol/L is well within the accurate range of the meters and can be used to confidently diagnose DKA and monitor the patient’s response to treatment.
Conclusions
Despite the increasing body of knowledge indicating that measurement of serum BHB can aid in both diagnosis and management of DKA, a study conducted in 2014 indicated that although 89% of pediatric emergency medicine and critical care providers responding to a survey stated that they had a DKA protocol at their institution, 67% perceived no clinical advantage in the use of serum ketone measurements [10]. This suggests that evaluation of serum ketone monitoring during DKA management from a quality improvement and research perspective may be necessary before clinical adoption is widespread. The next iteration of DKA management guidelines should address the potential utility of serum ketone monitoring.
References
1. Wolfsdorf J, Craig ME, et al. Diabetic ketoacidosis in children and adolescents with diabetes. Pediatr Diabetes 2009; 10(Suppl 12): 118–133.
2. Sheikh-Ali M, Karon BS, et al. Can serum beta-hydroxybutyrate be used to diagnose diabetic ketoacidosis? Diabetes Care 2008; 31(4): 643–647.
3. Arora S, Henderson SO, et al. Diagnostic accuracy of point-of-care testing for diabetic ketoacidosis at emergency-department triage: {beta}-hydroxybutyrate versus the urine dipstick. Diabetes Care 2011; 34(4): 852–854.
4. Charles RA, Bee YM, et al. Point-of-care blood ketone testing: screening for diabetic ketoacidosis at the emergency department. Singapore Med J. 2007; 48(11): 986–989.
5. Ham MR, Okada P, White PC. Bedside ketone determination in diabetic children with hyperglycemia and ketosis in the acute care setting. Pediatr Diabetes 2004; 5(1): 39–43.
6. Noyes KJ, Crofton P, et al. Hydroxybutyrate near-patient testing to evaluate a new end-point for intravenous insulin therapy in the treatment of diabetic ketoacidosis in children. Pediatr Diabetes 2007; 8(3): 150–156.
7. Rewers A, McFann K, Chase HP. Bedside monitoring of blood beta-hydroxybutyrate levels in the management of diabetic ketoacidosis in children. Diabetes Technology & Therapeutics 2006; 8(6): 671–676.
8. Laffel LM, Wentzell K, et al. Sick day management using blood 3-hydroxybutyrate (3-OHB) compared with urine ketone monitoring reduces hospital visits in young people with T1DM: a randomized clinical trial. Diabet Med. 2006; 23(3): 278–284.
9. Wolfsdorf JI. The International Society of Pediatric and Adolescent Diabetes guidelines for management of diabetic ketoacidosis: Do the guidelines need to be modified? Pediatr Diabetes 2014; 15(4): 277–286.
10. Clark MG, Dalabih A. Variability of DKA management among pediatric emergency room and critical care providers: a call for more evidence-based and cost-effective care? J Clin Res Pediatr Endocrinol. 2014; 6(3): 190–191.
The authors
Angela M. Ferguson*1 PhD, DABCC, FACB; Jeffery Michael1 D.O., FAAP; Stephen DeLurgio2 PhD; Mark Clements1 MD, PhD, CPI
1Children’s Mercy Hospital, Kansas City, MO, USA
2Bloch School, University of Missouri, Kansas City, MO, USA
*Corresponding author
E-mail: amferguson@cmh.edu