Clinical labs: in the frontline of new respiratory epidemics
Simmering concerns about respiratory disease pandemics flared up again in mid-February after the death of a patient in Britain due to infection by a new coronavirus. The virus is part of a family which also includes the one that caused the deadly SARS (severe acute respiratory syndrome) crisis.
To recall, in the space of just seven months from November 2002, SARS spread from Hong Kong to over 37 countries, infecting over 8,000 people and killing 775. Its mortality rate was close to that of the 1918 Spanish flu outbreak – billed the ‘Mother of all Pandemics’, and 100 times more than typical influenza epidemics. SARS has since faded away, but the virus is probably lying dormant; it can also infect cats and dogs.
SARS, bird flu and swine flu
SARS outgunned the H5N1 influenza strain which also emerged out of Asia in 1997; this was largely due to the inability of the latter, best known as ‘bird flu’, to spread between people.
In 2009, another influenza strain, Type A/H1N1, involving a cocktail of genes from pigs, birds and humans, was identified in Mexico. By June, the World Health Organization (WHO) had declared the disease (dubbed ‘swine flu’) as a Level 6 pandemic , but this was due to the speed of its spread rather than mortality, which was less than the common flu.
The new coronavirus
The numbers infected by the new coronavirus are small, just 12, so far. However, the virus has some troubling characteristics. Unlike swine flu, mortality is high, and typically accompanied by pneumonia and renal failure. Of the 12 infected so far, six have died, according to the WHO. Of equal concern is the possibility of human-to-human transmission, as opposed to bird flu.
This time, the new virus has its origins in the Middle East, with Saudi Arabia and Jordan accounting for seven infections and five deaths. In November 2012, the WHO reported cases from within one Saudi Arabian family. However, it was impossible to determine if the patients were infected separately but simultaneously (during travel), or whether the disease had spread between them. Europe hosts the remaining cases – one in Germany and four in Britain, including the Birmingham fatality. While the German patient had been in Qatar, in Britain, rather than the victim, it was his father who had travelled to the Middle East. Since then, the father is reported to have infected yet another family member. Prof. John Watson, head of the Respiratory Disease Unit at the British Health Protection Agency (HPA), noted that this suggested “that person-to-person transmission has occurred.”
Nevertheless, British health officials have been quick to ward off panic. The Birmingham victim is reported to have had a weakened immune system placing him in a vulnerable risk group. The HPA’s Deputy Chief Executive Dr. Paul Cosford has underlined that the disease appears “very difficult to catch.” Prof. Wendy Barclay of Imperial College London adds: “We’re an incremental step closer to worrying, but it isn’t a worry where we need to say there is a pandemic coming.”
Getting it right
These are reassuring words for the public, but hardly so for clinical laboratories. If any of the above assumptions are (or turn out to be) wrong, the challenge for labs will be herculean – as demonstrated during the SARS crisis. Indeed, Prof. Barclay’s statements were reported four days before the new virus took its first casualty in Britain.
Though coronaviruses are fragile (they are easily destroyed by detergents and survive outside a host organism for only a day or so), the severity of illnesses like SARS compel authorities to err on the side of caution – including enforcing quarantine (with its disturbing legal implications). The nature of such a response, in turn, places inordinately heavy demands on labs to get their diagnoses right, and be ready to ramp up scale exponentially. Complicating matters further is the fact that coronaviruses are a large family. Other than SARS, they also include the virus which causes the common cold.
Though several diagnostic tests have emerged since the SARS crisis, each has its limitations. Enzyme-linked immunosorbent assays (ELISA) detect antibodies to SARS reliably, but only 21 days after the onset of symptoms. Immunofluorescence assays (IFA) take half the time but require an immunofluorescence microscope and highly skilled staff. Polymerase chain reaction (PCR) tests are extremely specific, but less sensitive: though positive results strongly indicate SARS infection, negative results do not necessarily mean its absence.
Guidelines for respiratory disease epidemics
The WHO’s laboratory guidelines for SARS hint at the magnitude of the challenge of any new respiratory disease epidemic. Above all, its recommendations on interpreting results are cumbersome. Positive PCR requires at least two different clinical specimens from a patient, or the same specimen collected on two or more days, or two different assays or repeat PCR using the original clinical sample on each occasion of testing.
For ELISA and IFA testing, the WHO specifies a negative antibody test on acute serum, followed by a positive antibody test on convalescent serum, or an over four-fold rise in antibody titre between the acute and convalescent phase
sera, which must be tested in parallel.
So far, evidence of the origin of the new Middle Eastern coronavirus is sketchy. Genetic sequencing at a Dutch laboratory has established that the virus is not the one which causes SARS. Since then, phylogenetic analysis has shown its closest relatives are bat coronaviruses from Hong Kong.
Labs: frontline defence and court of last resort
A Health Canada study titled ‘Learning from SARS’ is an excellent evaluation of the role of laboratories – above all, that of lab personnel, during the crisis. One conclusion was that though the country’s Winnipeg-based National Microbiology Laboratory (NML) was “not designed for an epidemic response”, its personnel (and those from labs across the country) managed to quickly and effectively move into crisis management mode.
The study highlighted the unique role of laboratories as both a ‘first-line’ defence against a new threat as well as a ‘court of last resort’ to improve testing – in terms of diagnosis, surveillance, and response to epidemics.
One priority, according to the Health Canada study, is to standardize testing protocols and share data, to “see the whole picture” of an evolving epidemic. This, it argued, required laboratory information systems (LIS) that are “agile, modular, and rapidly modifiable for special purposes“, a lesson which has relevance for LIS designers even today. On its part, the WHO has mentored an international network of laboratories to identify best practices from the SARS
experience. This will clearly have a bearing on preparations for any new epidemic.
The impact of air travel
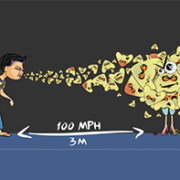
The challenge of respiratory system viruses is emphasized by the huge numbers of air travellers. Though little research has been done on the role of airplanes in respiratory epidemics, circumstantial evidence is strong. When SARS struck, 16 of 120 people on a single flight from Hong Kong to Beijing developed the disease, from just one index case. Conversely, the fall in air travel after the September 2011 US terror attacks sharply reduced flu incidence during the year.
Today, of some 8 million air passengers aloft every day, over 1 million cross international borders, just like the victims of the new virus in Britain and Germany. This is an area clearly in need of official attention. Indeed, in March 2003, the WHO recommended screening airline passengers for SARS but its impact was minimal, and questionable. Given the massive number of air travellers, it is clear that any new respiratory epidemic will first grow by leaps and bounds before any meaningful steps can be devised to control it.
The promise of biosensors
Some experts believe that airports should be provided with the means (and the authority) to screen passengers in an impending epidemic, for alternative causes. During the SARS crisis, such eliminative tests – even in a sophisticated setting like the US – were “ordered at the discretion of local clinicians”, diagnosed on “the basis of local interpretations” and many “were never reported to CDC.”
Today, at least one handheld, biosensor-based kit for diagnosing influenza A and B and respiratory syncytial viruses (RSV) – without having to send samples to the lab – is close to market. Deploying such devices at airports ought to be the next step, given the potential threat from the new Middle Eastern coronavirus as well as others that may arise in the future.
This would free laboratories to concentrate on their main task – to identify and confirm genuine, high-risk cases and direct their expertise to what Health Canada billed as their role as a ‘court of last resort’: to quickly master new diagnostic techniques and ensure a quicker response to containing epidemics.