Diagnosis of blood-borne parasitic infections: an overview
Methods for the diagnosis of blood-borne parasitic infections have stagnated in the last 20–30 years. However, recently, there has been a tremendous effort to focus research on the development of newer diagnostic methods focusing on serological, molecular, and proteomic approaches. This article examines the various diagnostic tools that are being used in clinical laboratories, optimized in reference laboratories and employed in mass screening programmes.
by A. Ricciardi and Dr M. Ndao
Blood-borne protozoans are the causative agents of some of the world’s most devastating and prevalent parasitic infections. This group of pathogens includes members of the Trypanosoma, Leishmania, Plasmodium, Toxoplasma, and Babesia genera. Most of these infections, with the exception of toxoplasmosis and babesiosis, have always been described as being tropical or subtropical. However, the increase in international travel as well as the arrival of new immigrants has made some of these tropical diseases realities in developed countries as well. In addition, infection via contaminated blood (transfusions and organ transplants) has become a major problem. Clearly, the transmission of blood-borne protozoans is boundless and the actual number of cases is underestimated. Quick diagnosis has always been a priority in order to determine the appropriate treatment and prevent fatalities. In addition, now more than ever, advances in diagnostics can help prevent transmission and provide active surveillance. Currently, diagnostic and reference laboratories use an array of techniques including microscopy, serological assays, and molecular assays. Here, the advantages and disadvantages of the methods will be discussed.
Toxoplasmosis
Toxoplasmosis, caused by Toxoplasma gondii, has a worldwide distribution. In immunocompetent individuals, more than 80% of primary Toxoplasma infections are asymptomatic [1]. Toxoplasmosis becomes a problem when an individual is immunocompromised or during pregnancy. Diagnosis of toxoplasmosis varies according to the immune status of the patient.
Diagnosis of immunocompetent individuals relies on serology. Early antibody responses can be detected via methods such as the dye test, immunofluorescent assay, and agglutination test whereas later IgG titres are detected by enzyme-linked immunosorbent assay (ELISA). For many years, the Sabin-Feldman dye test was the gold standard diagnostic technique due to its sensitivity and specificity. In recent years, few laboratories have continued to use this method and rather focused on newer techniques such as indirect immunofluorescent antibody tests, hemagglutination tests, capture ELISAs, and immunosorbent agglutination assays (ISAGAs). Serological assays lack the capacity to differentiate between recent and older infections; IgM levels can persist for over two years [2]. In order to determine whether an infection is recent, avidity ELISA is performed. This assay verifies IgG avidity and is based on the concept that as the immune response progresses, an immunoglobulin’s affinity for a specific antigen will increase [3].
Diagnosis of Toxoplasma infection during pregnancy is crucial in order to prevent congenital toxoplasmosis. Prenatal diagnosis involves performing real-time polymerase chain reaction (PCR) using amniotic fluid. The PCRs used often target the B1 gene of the parasite [1]. Upon delivery, PCR is performed on either the placenta or the cord blood serum in order to detect parasites. ISAGAs are also often performed. If the tests are positive, cord blood samples at one week of life are sent to a reference laboratory [1]. Follow up serology is again performed at one month and then every two to three months. There have been recent advances in the field of toxoplasmosis post-natal diagnosis. An ELISA assay that measures interferon-gamma levels upon stimulation of whole blood cells with Toxoplasma crude antigens has been developed. This method has proven to be both sensitive and specific [4].
In the case of immunocompromised patients, a quick diagnosis is essential because the infection can be fatal. Diagnosis relies on detecting parasites either by PCR or microscopy. Microscopic examination of Giemsa-stained tissues or smears is the quickest and most inexpensive method for diagnosing toxoplasmosis. However, poor sensitivity is the major pitfall of this method. PCR can also be performed on blood or cerebral spinal fluid (CSF) samples in order to detect parasite DNA. However, the degree of sensitivity attained by the PCRs is questionable and requires further investigations [1].
Leishmaniasis
Protozoans of the Leishmania genus are transmitted to humans via sand fly bites. Visceral leishmaniasis (VL), which is a lethal infection if left untreated, can also be transmitted by blood transfusions, organ transplants, and sharing of needles among intravenous drug users.
Direct parasitological methods, such as microscopy and cultures, are the gold standard methods when diagnosing VL. These methods have high specificity, but varying sensitivity. Direct detection of parasites is performed by microscopic examination of aspirates from spleen, bone marrow, or lymph nodes [5]. Using spleen samples increases sensitivity, but the procedure to obtain the aspirates risks internal bleeding. Parasite culturing from aspirates is widely used by reference laboratories.
Extensive research on the development of Leishmania serological assays has uncovered a myriad of candidate diagnostic antigens. The most promising antigens were the kinesin-related proteins. From this group, rK39 was the most tested antigen [6–8]. The rK39 antigen has been used to develop an immunochromatographic strip test (ICT)-based rapid diagnostic test which is advantageous for mass screening in endemic areas. This test requires a drop of peripheral blood and can be completed in approximately fifteen minutes [7]. Although the rK39 ICT rapid test was quite successful in Asia, it was often unable to detect Leishmania infections in African patients [5]. Additionally, rapid diagnostic tests still need standardization in order to become a regular practice in clinical laboratories.
PCR is the main molecular tool for Leishmania diagnosis due to its high sensitivity and reliability. Different PCR target sequences that are commonly used include ribosomal RNA genes, kinetoplast DNA, mini-exon derived RNA, internal transcribed spacer regions, etc., [5]. Quantitative PCR is useful because it allows for the quantification of parasites as well as species typing. Furthermore, this technique can be used to monitor treatment efficiency. Unfortunately, equipment requirements as well as the high cost limit the use of PCR for mass screening purposes in the field. The introduction of loop-mediated isothermal amplification (LAMP) could facilitate the use of molecular techniques for diagnostics. LAMP is highly specific, carried out under isothermal conditions, quick, and requires less complicated equipment (5). Moreover, reagents can be kept at room temperature, and there are no post-PCR steps. Assessment of drug treatment can also be carried out through the use of nucleic acid sequence based amplification (NASBA) which amplifies RNA sequences under isothermal conditions. Coupled to oligochromatography, NASBA can be used to monitor the progression from active disease to cure [9].
Chagas Disease (American Trypanosomiasis)
Chagas disease is the result of an infection with the blood-borne protozoan Trypanosoma cruzi. The parasite is transmitted by the triatomine bug. The second most important mode of transmission is via contaminated blood. This includes blood transfusions, organ transplants, and congenital transmission.
During the acute stage of Chagas disease, parasites can be observed in the blood. For this reason, diagnosis is carried out by direct microscopic viewing of Giemsa-stained thin and thick blood smears [10]. Parasites may also be detected through the use of hemocultures. In Chagas endemic areas, xenodiagnosis may be performed. This method involves allowing the naïve triatomine bug to take a blood-meal from the patient, and then analysing the bug for the presence of trypanosomes. It is believed that with continued research, molecular methods will eventually replace indirect diagnostic techniques such as blood cultures and xenodiagnosis [10]. However, molecular tests need to be standardized for routine clinical practice.
During the chronic stage of Chagas disease, diagnosis relies on serology; however, these tests often yield results that are difficult to interpret [10]. Commonly used, standardized serological assays include indirect immunofluorescence (IIF), indirect hemagglutination (IHA), and ELISA. IIF and IHA are commonly used due to their good sensitivity; however, their results are operator-dependent, and there is a lack of studies which analyse their reproducibility [10]. Currently, the immunoblot and radioimmunoprecipitation assays are in the process of being standardized. Both tests showed promise in early studies. A great deal of work is also being focused on the development and standardization of molecular methods such as PCR, which could be useful in monitoring chronic phase, reactivation, and treatment response.
As previously mentioned, disease transmission can also occur from mother to child, leading to congenital Chagas. Screening of neonates can be performed via direct methods, such as microscopy, or PCR using venous or cord blood samples from the newborn. These tests have very high sensitivity when performed during the first month of life [10]. Serological analysis may also be performed.
Sleeping Sickness (African Trypanosomiasis)
Trypanosoma brucei is the causative agent of African trypanosomiasis, and it is transmitted via the bite of the tsetse fly. During the first stage of the disease, parasites can be found circulating in the peripheral blood. The second stage is marked by parasites crossing the blood-brain barrier and infecting the central nervous system (CNS). The parasitic subspecies dictates geographic distribution, prognosis, and diagnosis.
T. b. gambiense causes West African trypanosomiasis, which is a slow progressing disease and is characterized by low parasite loads [11]. Definite diagnosis is carried out by microscopic observation of blood, lymph node aspirate, or CSF for the presence of parasites. In the field, the card agglutination test for trypanosomiasis (CATT/T. b. gambiense) has been widely used since its development in 1978 (12). Whole blood is used, and the assay directly detects T. b. gambiense specific antibodies. CATT/T. b. gambiense is cheap, quick, and highly sensitive. However, the test can give rise to false positives in individuals who are co-infected with malaria [12]. Although CATT/T. b. gambiense is the most sensitive, similar tests such as micro-CATT and LATEX/ T. b. gambiense can also be used. If these assays generate positive results, they need to be confirmed by microscopy or other molecular methods.
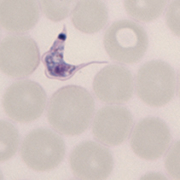
T. b. rhodesiense causes East African trypanosomiasis, which progresses quickly and is characterized by high parasite loads (11). For this subspecies, there is no diagnostic equivalent to the CATT/T. b. gambiense. However, diagnosis by microscopic observations of thick and thin smears is simple due to the elevated parasite load associated with T. b. rhodesiense.
Microscopy is the most practical technique to be used in rural areas. However, microscopy requires adequately qualified personnel in order to prevent misdiagnosis. Molecular methods would substantially improve the diagnosis of African trypanosomiasis. PCR techniques have been developed to screen the CSF of patients. The discovery of the SRA gene in T. b. rhodesiense has proven to be a breakthrough for the promotion of PCR techniques. Reactions targeting this gene have the potential to identify a single trypanosome [11]. There has also been the introduction of fluorescence in-situ hybridization in combination with peptide nucleic acid probes aimed towards ribosomal RNA. However, these tools for diagnosis are new and require further optimization. Extensive research is being focused on standardizing molecular techniques and rendering them more accessible. The use of LAMP is a step forward in improving molecular
approaches [11].
Future research needs to focus on the improvement of molecular diagnostic techniques. Currently, second stage infections are diagnosed by microscopic observation of CSF. Research is being conducted to test various cytokines and antibodies as biomarkers for CNS infection [11].
Malaria
Malaria is the most important parasitic infection in the world due to its high mortality. The causative agents, parasites of the Plasmodium genus, are transmitted by Anopheles mosquitoes. Quick diagnosis is essential in order to determine the appropriate treatment as well as to prevent further transmission.
Microscopy is the gold standard for laboratory diagnosis. This method involves detecting parasites in Giemsa-stained thick and thin blood smears. However, microscopic results are operator-dependent, thereby causing the sensitivity to vary. A great deal of effort has been focused on developing rapid diagnostic tests (RDTs) which can be used in the field. These tests can supplement microscopy, but they cannot replace it yet. Current RDTs are serology based and use three different Plasmodium antigens: Plasmodium histidine-rich protein, Plasmodium lactate dehydrogenase, or Plasmodium aldolase [13]. These tests are quick, easy to perform, and require minimal patient samples. However, they are not specific for species such as P. malariae, P. ovale, and P. knowlesi. Furthermore, false positives may be observed due to cross-reactions in patients with Schistosoma mekongi or rheumatoid factor [14]. In addition, the tests inefficiently detect P. falciparum infections from South America, as this species does not produce the common histidine-rich proteins [15].
Currently, there are no commercially available molecular assays. Although some reference and government laboratories have developed their own molecular assays, their availability is limited. LAMP is currently in the spotlight. Poon et al. developed a LAMP test which detected the target sequence of P. falciparum 18S ribosomal RNA gene [16]. They stated that the price of this test was one tenth that of a conventional PCR. Recently, LAMP was further simplified in the form of a card test. It was used in combination with DNA filter paper and melting curve analysis. This system was shown to be highly specific and sensitive [17]. Improvement of the LAMP technique should be geared towards the development of rapid diagnostic tests which could potentially be used in the field.
Babesiosis
Babesiosis is caused by parasites belonging to the Babesia genus that are spread by certain ticks commonly found in North America. The parasites infect red blood cells (RBCs), and consequently cause hemolytic anemia. The disease can be fatal in splenectomy patients, immunocompromised individuals, and the elderly. Diagnosis is complicated by the symptoms’ resemblance to other tick-borne illnesses.
The gold standard of babesiosis diagnosis relies on detecting the parasites in the patients’ RBCs. This is achieved by microscopic observation of thick and thin blood smears. Babesia infections can be easily mistaken for P. falciparum infections [18]. Additionally, false negatives are common in immunocompetent individuals whose parasitemia can be lower than 1% [18]. Samples are often sent to reference laboratories in order to confirm ambiguous results. IFFs are used to detect anti-babesial IgM and IgG [18]. They are sensitive, specific, and reliable. ELISAs and immunoblots, although not standardized, can be performed to confirm the IFF results. However, compared to IFFs, Babesia detecting ELISAs require higher concentrations of antigen and have varying sensitivity [18]. Future research on babesiosis diagnosis is aimed at developing multiplex PCR assays that will be able to detect several tick-borne infections. PCR assays have the potential to yield positive results from 100µl blood samples containing as little as three parasites; demonstrating the incredible advantage that molecular techniques could contribute to diagnosis of this parasitic disease [18].
Proteomics
Dr Momar Ndao’s laboratory focuses on the improvement and advancement of diagnosis. Through our work, we hope to encourage the development of proteomic strategies for the diagnosis of parasitic infections. Mass-spectrometry platforms are the future of proteomics, and they can be used to identify biomarkers from biological fluids. Some techniques that can be used to analyse protein expression include matrix-assisted laser desorption ionization time-of-flight mass-spectrometry (MALDI-TOF MS), surface-enhanced laser desorption ionization time-of-flight mass-spectrometry (SELDI-TOF MS), liquid chromatography combined with mass-spectrometry, isotope-coded affinity tags, and isobaric tags for relative and absolute quantification [19]. When SELDI is used, samples are directly spotted onto chemically active ProteinChip Array surfaces which can be chosen based on specific chemical and biological properties. With MALDI, samples are mixed with the matrix component prior to loading on a chip. These proteomic platforms can be useful in identifying biomarkers that are indicative of a specific pathophysiological state. Currently, members of our laboratory are using both SELDI and MALDI techniques extensively to identify biomarkers of blood borne parasites.
Summary
Quick and correct diagnosis of parasitic infections is crucial to avoid deaths and further disease transmission. Diagnostic methods include parasitological techniques, such as microscopy and culturing, serological assays, and molecular tests [Table 1]. Although several serological and molecular diagnostic tools are being tested and used by certain reference laboratories, results are always confirmed by microscopy which remains the gold standard. Many newer assays have not been standardized yet, thus, forcing diagnosticians to rely on microscopic observations. Unfortunately, the evolution of diagnosis in the field of parasitology has been slow to progress. Fortunately, in recent years, several groups have focused their research on the improvement of diagnostics. Current research emphasizes the development and optimization of molecular techniques such as PCR and LAMP. Additional work must concentrate on rendering molecular diagnostics more accessible. Although relatively new at the moment, proteomic platforms seem to be the future of diagnosis. These new techniques can identify biomarkers which can categorize susceptible individuals, distinguish between the different stages of an infection, and monitor whether treatments lead to cure. Diagnostic research has made much progression, however, there is still a lot of work to be done and improvements to be made. In order to better the diagnosis of blood-borne parasitic infections, research plus communication is the answer.
References
1. Robert-Gangneux F and Darde ML. Clin Microbiol Rev 2012; 25: 264–96.
2. Gras L, et al. Epidemiol Infect 2004; 132: 541–8.
3. Lefevre-Pettazzoni M, et al. I Clin Vaccine Immunol 2007; 14: 239–43.
4. Chapey E, et al. J Clin Microbiol 2010; 48: 41–5.
5. Srividya G, et al. Parasitol Res 2012; 110: 1065–78.
6. Badaro R, et al. J Infect Dis 1996; 173: 758–61.
7. Chappuis F, et al. Trop Med Int Health 2006; 11: 31–40.
8. Singh S, et al. Clin Diagn Lab Immunol 2002; 9: 568–72.
9. Saad AA, et al. PLoS Negl Trop Dis 2010; 4: e776.
10. Lescure FX, et al. Lancet Infect Dis 2010; 10: 556–70.
11. Welburn SC, et al.. Adv Parasitol 2012;79: 299–337.
12. Magnus E, et al. Ann Soc Belg Med Trop 1978; 58: 169–76.
13. Wilson ML. Clin Infect Dis 2012; 54: 1637–41.
14. Leshem E, et al. J Clin Microbiol 2011; 49: 2331–2.
15. Gamboa D, et al. PLoS One 2010; 5: e8091.
16. Poon LL, et al. Clin Chem 2006; 52: 303–6.
17. Yamamura M, et al. Jpn J Infect Dis 2009; 62: 20–5.
18. Hunfeld KP, et al. Int J Parasitol 2008; 38: 1219–37.
19. Ndao M. Interdiscip Perspect Infect Dis 2009; 2009: 278246.
The authors
Alessandra Ricciardi, BSc
National Reference Centre for Parasitology, Research Institute of the McGill University Health Center, Montreal, Canada
Momar Ndao, DVM, MSc, PhD
National Reference Centre for Parasitology at the Montreal General Hospital, Montreal, Quebec, Canada
E-mail: momar.ndao@mcgill.ca