Autoantibodies against MDA-5: very important serological markers in amyopathic dermatomyositis with rapidly progressive interstitial lung disease
Autoantibodies against MDA-5 are serologically important biomarkers because they are mainly detected in patients with amyopathic dermatomyositis complicated with rapidly progressive interstitial lung disease (ILD). Anti-MDA-5 antibodies are useful not only for diagnosis but possibly also for monitoring disease activity in ILD.
by Assoc. Prof. Y. Muro, Assoc. Prof. K. Sugiura and Prof. M. Akiyama
Dermatomyositis and autoantibodies against melanoma differentiation-associated gene 5
Idiopathic inflammatory myopathies (IIMs) are a group of systemic autoimmune diseases that include polymyositis (PM), dermatomyositis (DM) and inclusion body myopathies [1]. Several myositis-specific autoantibodies (MSAs) are associated with certain clinical forms of IIMs, and they are useful tools for predicting the prognosis of IIMs. For example, patients that are positive for anti-transcriptional intermediary factor 1-gamma (TIF1-γ) antibodies are often complicated with internal malignancies, and patients that are positive for anti-melanoma differentiation-associated gene 5 (MDA-5) antibodies demonstrate rapid progressive interstitial lung disease (ILD) [2]. Since these complicating diseases are life-threatening, the above antibodies are very important biomarkers.
Many recent studies have clarified new MSAs which are associated with clinical subsets of DM/PM. As MSAs are basically mutually exclusive, they also can be used to determine the disease subset. A subgroup of DM patients is known to have typical skin manifestations of DM but with little evidence of myositis, a condition known as clinically amyopathic DM (ADM). Initially, anti-MDA-5 antibodies were reported to be serological markers of clinically ADM with rapidly progressive ILD, especially in East Asia; they also are found in Caucasian patients with ADM complicated with ILD. A Japanese multicentre study found the 5-year survival for patients with anti-MDA-5 antibodies to be 56% [3].
Function of MDA-5
The MDA-5 gene was originally identified as an upregulated sequence in a cDNA subtraction library screening of terminally differentiating HO-1 human melanoma cells by combined treatment with IFN-β and mezerin [4]. The innate immune system senses RNA virus infections through membrane-bound toll-like receptors or the cytoplasmic proteins RIG-I and MDA-5 [5]. RIG-I and MDA-5 proteins comprise an amino-terminal caspase recruitment domain (CARD) and a carboxyl-terminal RNA helicase-domain. These sensors interact with a CARD-containing adaptor protein, IPS-1, located in the outer membrane of mitochondria after binding viral RNA. This interaction mediates recruitment and activation of protein kinases that phosphorylate the transcription IFN-regulatory factor 3, leading to the synthesis of type I IFN. RIG-I is essential for detecting infection by rhabdoviruses, influenza viruses, paramyxoviruses, and flaviviruses. Replication of these viruses leads to the production of RNAs with a 5’-triphosphate. In contrast, MDA-5 senses infection by picornaviruses and long-strand dsRNA. The mechanism for the discrimination of RNA ligands by RIG-I and MDA-5 is unknown. In a large screening of single-nucleotide polymorphisms associated with type 1 diabetes, a number of mutations in the MDA-5 gene were reported.
Discovery of anti-MDA-5 antibody
Anti-MDA-5 antibody was initially named anti-CADM-140 antibody before the recognized antigen was clarified [6]. CADM is an abbreviation of ‘clinically amyopathic dermatomyositis’, and the molecular size on SDS-PAGE is 140 kDa, as shown by immunoprecipitation. In 2009 and 2010, two independent groups identified MDA-5 as its autoantigen by cDNA expression library immunoscreening or by peptide mass fingerprinting [7, 8]. The common clinical features of patients with anti-MDA-5 in both studies were those typical of ADM (i.e. dermatomyositis with scarce manifestation of myositis), frequent complication of ILD and poor prognosis.
Detection of anti-MDA-5 antibodies
Indirect immunofluorescence assay using HEp-2 cells as the substrate is the most commonly used routine test for the detection of anti-nuclear/cytoplasmic autoantibodies. However, anti-MDA-5 antibodies show weak cytoplasmic pattern or frequently negative results. Although radioisotope-based immunoprecipitation assays have tended to be used to detect anti-MDA-5 antibodies, such assays are not easy to perform. Sato et al. established an ELISA for anti-MDA-5 antibodies by using recombinant protein produced by a baculovirus expression system [7]. To date, commercially available immunoassay kits that may clarify the unknown clinical significance of anti-MDA-5 across races or countries do not exist. It should be noted that anti-MDA-5 antibodies in patients do not react to RIG-I [7].
Longitudinal study of anti-MDA5
Systemic lupus erythematosus is also an autoimmune rheumatic disease that is characterized by a fluctuating disease course and a variety of autoantibodies. Many autoantibody specificities (SS-A/Ro, SS-B/La, Sm, U1-RNP) in lupus patients remain constant over time, whereas reactivity to dsDNA may fluctuate with disease activity, although the pattern of change differs with autoantibody specificity [9]. We established a quantitative assay of antibody levels and monitored anti-MDA-5 autoantibodies during long-term follow-up periods in order to assess the long-term outcome of ADM patients with anti-MDA-5 antibodies [10]. Our ELISA used biotinylated recombinant protein expressed by an in vitro transcription and translation system and streptavidin-coated plates. The levels of anti-MDA-5 were measured at different time points in 11 ADM patients who tested positive for anti-MDA-5 on their first visit (range of follow-up: 3 months to 16 years). At the stage of clinical remission of ADM+ILD, 6 of the patients received no medication and the 4 others received low-dose corticosteroid. One patient passed away due to rapidly progressive ILD. Surprisingly, the anti-MDA-5 antibodies disappeared in 9 of the patients and fell to just above the cut-off in 1 patient, whereas in the patient who died, the antibodies remained, as shown by ELISA.
Case report
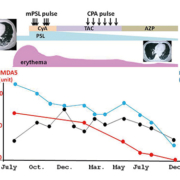
Gono et al. showed that the decline index of the anti-MDA5 level after treatment was lower in patients who died than in patients who survived [11]. We also recently came across an anti-MDA5-positive DM patient with ILD who showed a decrease in anti-MDA5 level before a fall in other biomarkers after therapy and favourable prognosis.
A 42-year-old Japanese man noticed erythema and papules on the dorsal surfaces of his hands in June and later erythema also on the face, neck and back. In July, he consulted a general practitioner, was suspected of having a collagen disease and was referred to our hospital. He had facial erythema and Gottron’s sign (i.e. erythema with slight scaling over the metacarpophalangeal and proximal interphalangeal finger joints). No muscle weakness was found, and the creatine kinase level was within the normal range. Although he noticed slight dyspnea upon exertion, interstitial changes to both lower-lung fields were seen by computed tomography. Our ELISA showed him to be positive for anti-MDA-5 antibodies, and various immunosuppressive agents were used for therapy (Fig. 1). He showed a decrease in anti-MDA-5 level before falls in other biomarkers (ferritin, SP-D) after intensive immunosuppressive therapy. He has now been under observation by our hospital on a minimum maintenance dose of prednisolone (5 mg/day).
Conclusions and future
In the previous studies [11, 12], anti-MDA-5 levels were higher in patients who later died than in patients who survived, but the difference in levels was not statistically significant. Although we agree that the anti-MDA-5 level is useful for the evaluation of response to treatment in ILD with ADM, it should be stressed that single-point evaluation of anti-MDA-5 level has limitations in predicting the prognosis of these patients. Other factors, such as the anti-MDA-5 isotype, in predicting the prognosis of these patients remain to be clarified. Commercially available immunoassay kits will be helpful for the investigation, as well as the monitoring, of each patient.
Not only is the anti-MDA-5 antibody a diagnostic marker of ADM+ILD, but it is also useful as an indicator for response to therapy. Considering that MDA-5 plays important roles in the innate immune system during RNA viral infections, an autoantigen/autoantibody system of MDA-5 should be linked to the pathogenesis of this disease condition. For example, MDA-5 was shown to be degraded in cells infected with different picornaviruses [13]. Whether such cleavage might lead to autoimmune responses against MDA-5 (i.e. antigen-driven) needs investigation.
References
1. Mammen AL. Dermatomyositis and polymyositis: Clinical presentation, autoantibodies, and pathogenesis. Ann N Y Acad Sci. 2010; 1184: 134–153.
2. Hoshino K, Muro Y, Sugiura K, Tomita Y, et al. Anti-MDA5 and anti-TIF1-γ antibodies have clinical significance for patients with dermatomyositis. Rheumatology 2010; 49: 1726–1733.
3. Hamaguchi Y, Kuwana M, Hoshino K, Hasegawa M, et al. Clinical correlations with dermatomyositis-specific autoantibodies in adult Japanese patients with dermatomyositis: a multicenter cross-sectional study. Arch Dermatol. 2011: 147: 391–398.
4. Jiang H, Fisher P. Use of sensitive and efficient subtraction hybridization protocol for the identification of genes differentially regulated during the induction of differentiation in human melanoma cells. Mol Cell Different. 1993; 1: 285–299.
5. Barral PM, Sarkar D, Su Z-Z, Barber GN, et al. Functions of the cytoplasmic RNA sensors RIG-I and MDA-5: key regulators of innate immunity. Pharmacol Ther. 2009; 124: 219–234.
6. Sato S, Hirakata M, Kuwana M, Suwa A, et al. Autoantibodies to a 140-kd polypeptide, CADM-140, in Japanese patients with clinically amyopathic dermatomyositis. Arthritis Rheum. 2005; 52: 1571–1576.
7. Sato S, Hoshino K, Satoh T, Fujita T, et al. RNA helicase encoded by melanoma differentiation-associated gene 5 is a major autoantigen in patients with clinically amyopathic dermatomyositis: Association with rapidly progressive interstitial lung disease. Arthritis Rheum. 2009; 60: 2193–2200.
8. Nakashima R, Imura Y, Kobayashi S, Yukawa N, et al. The RIG-I-like receptor IFIH1/MDA5 is a dermatomyositis-specific autoantigen identified by the anti-CADM-140 antibody. Rheumatology (Oxford) 2010; 49: 433–440.
9. Tench CM, Isenberg DA. The variation in anti-ENA characteristics between different ethnic populations with systemic lupus erythematosus over a 10-year period. Lupus 2000; 9: 374–376.
10. Muro Y, Sugiura K, Hoshino K, Akiyama M. Disappearance of anti-MDA-5 autoantibodies in clinically amyopathic DM/interstitial lung disease during disease remission. Rheumatology (Oxford) 2012; 51: 800–804.
11. Gono T, Sato S, Kawaguchi Y, Kuwana M, et al. Anti-MDA5 antibody, ferritin and IL-18 are useful for the evaluation of response to treatment in interstitial lung disease with anti-MDA5 antibody-positive dermatomyositis. Rheumatology (Oxford) 2012; 51: 1563–1570.
12. Muro Y, Sugiura K, Akiyama M. Limitations of a single-point evaluation of anti-MDA5 antibody, ferritin, and IL-18 in predicting the prognosis of interstitial lung disease with anti-MDA5 antibody-positive dermatomyositis. Clin Rheumatol. 2013; 32: 395–398.
13. Barral PM, Morrison JM, Drahos J, Gupta P, et al. MDA-5 is cleaved in poliovirus-infected cells. J Virol. 2007; 81: 3677–3684.
The authors
Yoshinao Muro* MD, PhD; Kazumitsu Sugiura MD, PhD; and Masashi Akiyama MD, PhD
Division of Connective Tissue Disease and Autoimmunity, Department of Dermatology, Nagoya University Graduate School of Medicine, Nagoya, JAPAN
*Corresponding author
E-mail: ymuro@med.nagoya-u.ac.jp