Carbapenemases: a major threat to healthcare
Bacterial resistance to antibiotics is a major health and economic problem recognized today by national and international policy makers. The Enterobacteriaceae belong to the commensal human gut flora and are frequently the cause of community- and healthcare-associated infections (HAI). Infections with Klebsiella pneumoniae are usually hospital-acquired and occur primarily in patients with impaired host defences while Escherichia coli are mostly involved in urinary tract infections. Acinetobacter and Pseudomonas species are opportunistic pathogens frequently isolated from healthcare settings where they cause life-threatening infections particularly in immunocompromised patients.
For several years, in Europe and worldwide, Enterobacteriaceae, mainly K. pneumoniae and E. coli but also non-fermenting bacteria (Acinetobacter baumannii and ) have become resistant to the main antibiotics, i.e. ß-lactam antibiotics, fluoroquinolones and aminoglycosides [1]. In particular, the US “Center for Disease Control and Prevention” (CDC) pointed the carbapenemase-producing Enterobacteriaceae (CPE) (or Carbapenem Resistant Enterobacteriaceae, CRE) among the three microorganisms exhibiting the most urgent health risk. Carbapenemases are indeed enzymes that inactivate ß-lactam antibiotics like carbapenems that currently constitute the last resort for treating multi-drugs resistant Gram-negative bacteria. Moreover, production of carbapenemases in these bacteria is most often associated with the expression of additional resistance mechanisms to other classes of antibiotics such as aminoglycosides, fluoroquinolones and cotrimoxazole, leading to bacteria resistant to all available antibiotics, so-called pan-resistant bacteria [2].
Carbapenemases resistance
Carbapenems are a class of broad-spectrum ß-lactam antibiotics with very broad activity and have therefore become the empirical treatment of choice in countries where infections due to Extended-Spectrum ß-Lactamases-producing bacteria are common. Resistance to carbapenems in Enterobacteriaceae is linked to either decreased permeability because of porine alteration or loss combined with production of a ß-lactamase with poor carbapenemase activity or, more worryingly, to the enzymatic breakdown of the antibiotic by a carbapenem-hydrolyzing ß-lactamase [3].These so called carbapenemases can hydrolyse and hence deactivate several kinds of antibiotics ranging from penicillins to cephalosporins, monobactams and carbapenems.
The most frequent carbapenemases in Enterobacteriaceae reported in Europe belong to three molecular classes according to the Ambler classification:
– class A carbapenemases hydrolyse almost all ß-lactams including carbapenems. Klebsiella pneumoniae carbapenemase (KPC) are the most frequent enzymes of this group that show a very high spreading capability [4] . KPC, contrary to other class A ß-lactamase, is inhibited by boronic acid and its derivatives.
– class B carbapenemases, belonging to metallo-ß-lactamases, including Verona integron-encoded metallo-ß-lactamase (VIM), IMP and the New Delhi metallo-ß-lactamase-1 (NDM-1) can hydrolyse all ß-lactams but monobactams. These enzymes are inhibited in vitro by EDTA and dipicolinic acid that are used in confirmatory tests for the presence of metallo ß-lactamases (MBL). NDM is the most frequent MBL present in Enterobacteriaceae. Originally detected in the Asian subcontinent, NDM is now spreading worldwide and causing outbreaks in Western countries.
– class D carbapenemases including the OXA carbapenem-hydrolysing oxacillinases hydrolyse penicillins but show lower activity against carbapenems, and no activity against extended-spectrum cephalosporins [5)]. OXA-48 is the main enzyme of this family and is now spreading worldwide even in the community although only a few cases are reported in the USA. OXA-48 hydrolyses all penicillins including temocillin. The resistance to temocillin primarly evidenced by a Belgian group [6] is now recommended as a marker of the possible presence of OXA-48. Resistance to carbapenems in OXA-48-producing CPE is variable with minimal inhibitory concentration againt carbapenems varying between less than 0.5 µg/mL to more than 256 µg/mL. This mechanism is very difficult to detect and no confirmatory test currently exists as OXA-48 is not specifically inhibited by clavulanic acid, boronic acid or EDTA. To date, only expensive molecular tests are able to confirm the presence of OXA-48. The rapid and global expansion of CPE is a threat to healthcare and patient safety worldwide, as it seriously curtails the ability to cure infections. Infections due to CPE are associated with higher in-hospital morbidity and mortality [7].
Carbapenemases epidemiology
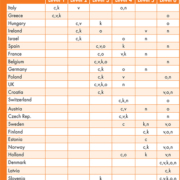
According to the report summarizing the results from 39 European countries [8], six levels of occurrence of CPE have been defined i.e. endemic situation (level 1), inter-regional spread (level 2), regional spread (level 3), sporadic hospital outbreaks (level 4), single hospital outbreaks (level 5) and sporadic occurrence (level 6).
Nevertheless, specific occurrence may also vary depending on the type of CPE.
Discussion
Carbapenemase-producing Enterobacteriaceae (CPE) are an emerging threat to healthcare and are frequently resistant to many other antibiotics besides carbapenems leaving few treatment options [9, 10]. Rapid diagnostic tests that can be performed directly on clinical specimens or blood cultures are urgently needed in order to save an average of 24 hours compared to the results obtained by culture. Some commercial tests of this type targeting carbapenemases from CPE currently exist and are based either on molecular amplification of specific genes associated with resistance or on molecular hybridization.
Some tests are able to target all carbapenemases of clinical interest, or other resistance mechanisms alongside with accurate species identification.
However, these tests require specific equipment and are extremely expensive (80 Euros being an average price).
Multiplex real-time PCR tests allow the detection of the genes encoding for the main carbapenemases directly from samples or feces but do not detect all variants of the genes of interest in a single operation.
Other molecular biology tests can be performed on isolated colonies from culture. These tests are costly (average cost of 40 €), quite labour-intensive and often do not deliver results before the next morning, when the susceptibility testing is already available. Molecular biology tests only partially meet the needs in carbapenemase identification. Either these tests do not cover the complete range of targets or cannot distinguish between different carbapenemases and, in any case, do not give information on the level of gene expression and thus the level of bacterial resistance. The high price of these techniques and/or the need for expensive equipment, dedicated areas and specially trained personnel restrict their use to a limited number of specialized laboratories.
Rapid phenotypic tests directly performed on bacterial colonies and based on the hydrolysis of a carbapenem with colorimetric shift are now available at a reasonable price. MALDI-TOF mass spectrometry is also proposed, however, this technology requires the use of expensive equipment together with specific software analysis. All the above phenotypic tests only partially meet the needs of clinical laboratories. On the one hand, most of them require the use of antibiotics with stability problems, and secondly, the time for obtaining a result with these tests is not totally satisfactory in terms of integration into the laboratory workflow that would ensure results in a short time and allow quick decision for optimal impact. On the other hand these phenotypic tests do not identify the exact type of carbapenemase and ideally require subsequent procedures using a molecular method to achieve identification. Among CPE, OXA-48 represents the most challenging resistance mechanism to be identified that would need a rapid and easy to use test to be performed in routine labs.
References
1. Carbapenemase-producing bacteria in Europe. Interim results from the European Survey on carbapenemase-producing Enterobacteriaceae (EuSCAPE) project 2013.
2. Souli M, Galani I, and Giamarellou H. Emergence of extensively drug-resistant and pandrug-resistant Gram-negative bacilli in Europe. Euro Surveillance 2008; 13(47).
3. Nordmann P, Naas T, and Poirel L. Global spread of carbapenemase producing Enterobacteriaceae. Emerging Infectious Diseases 2011; 17(10): 1791–1798.
4. Naas T, Cuzon G, Villegas M-V, Lartigue M-F, Quinn JP, and Nordmann P. Genetic structures at the origin of acquisition of the ß-lactamase blaKPC gene Antimicrobial Agents and Chemotherapy 2008; 52(4): 1257–1263.
5. Nordmann P, Naas T, and Poirel P. Global spread of carbapenemase producing Enterobacteriaceae. Emerging Infectious Diseases 2011; 17(10): 1791–1798.
6. Glupczynski Y, Huang TD, Bouchahrouf W, Rezende de Castro R, Bauraing C, Gérard M, Verbruggen AM, Deplano A, Denis O, Bogaerts P. Rapid emergence and spread of OXA-48-producing carbapenem-resistant Enterobacteriaceae isolates in Belgian hospitals. Int J Antimicrob Agents 2012; 39(2):168-72.
7. Borer A, Saidel-Odes L, Riesenberg K, Eskira S, Peled N, Nativ R, et al. Attributable mortality rate for carbapenem-resistant Klebsiella pneumoniae bacteremia. Infect Control Hosp Epidemiol 2009, 30:972–6.
8. Carbapenemase-producing Enterobacteriaceae in Europe: a survey among national experts from 39 countries, February 2013, Euro Surveill. 2013;18(28):pii=20525.
9. Cantón R, Akóva M, Carmeli Y, Giske CG, Glupczynski Y, Gniadkowski M, et al. Rapid evolution and spread of carbapenemases among in Europe, Clin Microbiol Infect. 2012;18(5):413–31.
10. Hawkey PM. The growing burden of antimicrobial resistance, J Antimicrob Chemother. 2008;62(Suppl 1):i1–i9.
The authors
Isabelle OTE, Laetitia AVRAIN, Pascal MERTENS, Thierry LECLIPTEUX
R&D Department, Coris BioConcept,
Parc Scientifique Crealys,
29A, rue Jean Sonet,
B-5032 Gembloux, Belgium