Combined PCT and MR-proADM testing in the diagnosis and prognosis of severe sepsis and septic shock
Early diagnosis of sepsis is essential for enabling appropriate treatment. PCT and MR-pro ADM have been shown to be independent biomarkers for sepsis and progression to septic shock, and simultaneous analysis seems to be more effective than the single marker approach.
by Dr S. Angeletti, M. De Cesaris, Dr A. Lo Presti, et al.
Introduction
Sepsis is a severe condition that represents the tenth most common cause of death in the USA. In Europe, sepsis occurs in more than 35% of the patients admitted in the intensive care unit. The mortality associated with sepsis is approximately 28% and it rises to 40–60% in cases of septic shock, despite adequate treatment administration. Nearly 9% of patients with sepsis experience severe sepsis and nearly 3% progress to septic shock leading to multi-organ failure. More than 50% of patients affected by septic shock do not survive [1–3]. Consequently, the rapid recognition and treatment of sepsis is mandatory to reduce both the mortality and the hospitalization with related costs [1-3].
Sepsis is commonly defined as the presence of infection in conjunction with the systemic inflammatory response syndrome (SIRS); severe sepsis, as sepsis complicated by organ dysfunction; and septic shock, as sepsis-induced acute circulatory failure characterized by persistent arterial hypotension despite adequate volume resuscitation and not explained by other causes [1, 4]. The diagnosis of sepsis and evaluation of its severity is complicated by the highly variable and non-specific nature of the signs and symptoms of sepsis [5]. However, the early diagnosis and stratification of the severity of sepsis is very important, increasing the possibility of starting timely and specific treatment [4, 6].
The gold standard for detection of bloodstream infections is blood culture. The time required for a positive blood culture result depends on the incubation time required for the culture to turn positive and the subsequent biochemical identification, along with an antibiotic sensitivity test, both of which usually take 48 h [7]. Furthermore, in some cases, blood culture results remain negative owing to empirical broad-spectrum antibiotics that are frequently started in the presence of SIRS and often continued for a prolonged time course despite the absence of clinical and microbiological data supporting a diagnosis of bacterial infection [4, 8]. Several studies have evaluated the diagnostic utility of various biomarkers, including ferritin, haptoglobin, interleukin 6, C-reactive protein (CRP) and procalcitonin (PCT) for suspected sepsis in the ICU patient population [9–11].
It remains difficult to differentiate sepsis from other non-infectious causes of SIRS [12] and there is a continuous search for better biomarkers of sepsis.
PCT is a polypeptide that has demonstrated the highest reliability in the early diagnosis of sepsis, severe sepsis or septic shock compared to other plasma biomarkers or clinical data alone [13]. Moreover, PCT has been advocated also to clarify the bacterial origin of some localized infections [14–15].
The mid-regional pro-adrenomedullin (MR-proADM) has been shown to play a decisive role in both the induction of hyper-dynamic circulation during the early stages of sepsis and the progression to septic shock [16–18], and recently it has been reported that MR-proADM differentiates sepsis from non-infectious SIRS with high specificity. Moreover, simultaneous evaluation of MR-proADM and PCT in septic patients increased the post-test diagnostic probabilities compared to the independent determination of individual markers [19–20]; probably the multimarker approach seems to be the more effective [14, 19].
The aim of the present study was to perform a focused evaluation of the role of the combination of PCT and MR-proADM in patients with severe sepsis and septic shock (SS) to differentiate it from patients with mild sepsis or SIRS for a prompt and specific treatment administration.
Methods
Patient and control characteristics
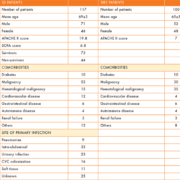
One hundred and seventeen patients with SS and 100 patients with SIRS, hospitalized at the University Hospital Campus Bio-Medico of Rome between the years 2012 and 2014, were enrolled in the study. The patients’ details are reported in Table 1.
Sepsis was defined by the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definition of sepsis [4] based on the presence of a recognized site of infection and evidence of a SIRS occurring when at least two of the following criteria are present: body temperature higher than 38°C or lower than 36°C, heart rate higher than 90 beats per minute, respiratory rate higher than 20 breaths per minute or hyperventilation as indicated by an arterial partial pressure of carbon dioxide (PaCO2) lower than 32 mm Hg and a white blood cell count of higher than 12,000 cells/mm3 or lower than 4,000.
Patients were classified according to clinical signs into SS and SIRS. Acute physiological and chronic health evaluation (APACHE) II and sequential organ failure assessment (SOFA) scores were computed. APACHE II scores in SS and SIRS patients were calculated by Medscape, APACHE II scoring system calculator [21]. The SOFA score was calculated only for SS patients to better define the severity of the sepsis [22–23]. The study was approved by the Ethics Committee of the University Hospital Campus Bio- Medico, Rome, Italy.
Blood culture
Blood samples for blood culture were collected when patients showed the symptoms and signs of SIRS [1, 2, 4]. Blood culture included three sets (time 0, time 30 and time 60 min) of one aerobic and one anaerobic broth bottles (Bactec Plus Aerobic/F, Bactec Plus Anaerobic/F, Beckton Dickinson) per patient drawn during 1-h period of clinically suspected bloodstream infection. Blood culture vials were incubated in the Bactec 9240 automated system (Beckton Dickinson). Blood culture samples that turned positive were immediately processed for Gram staining and cultivated. Bacterial identification was performed by MALDI-TOF, as previously described [24].
PCT and MR-proADM measurement
The plasma concentrations of PCT and MR-proADM were measured by an automated analyser using a time-resolved amplified emission method (Kryptor, Brahms AG), with commercially available assays (Brahms AG) [25].
Statistical analysis
Data was analysed using MedCalc 11.6.1.0 statistical package (MedCalc Software). Plasma levels of PCT and MR-proADM were log-transformed to achieve a normal distribution. The normal distribution of each marker concentration was tested by the Kolmogorov–Smirnov test. PCT and MR-proADM in patients with SIRS and SS were compared using the Mann–Whitney test. Multiple logistic regression analysis (stepwise method) using SS versus PCT and MR-proADM was performed and the odds ratio (OR) computed. For OR calculation variables were retained for P<0.05 and removed for P>0.1.
Receiver operating characteristic (ROC) analysis was performed among independent variables associated with SS to define the cut-off point for plasma PCT and MR-proADM and their diagnostic accuracy to predict SS [26]. Pre-test odds, post-test odds and the consequent post-test probability were computed to investigate whether the combination of PCT and MR-proADM improves post-test probability. Likelihood ratios were used as these tests are not prone to bias due to prevalence rates [27].
Results
Patients with SS and SIRS characteristics
The mean age of the 117 patients with SS (71 men and 46 women) was 69 ± 3 years (Table 1). The principal comorbidities of patients with SS and SIRS and the sources of bacteremia are summarized in Table 1. In patients with SS the average APACHE II score value was 19.8, corresponding to 24% risk of death and the average SOFA score was 6.8 corresponding to a predicted mortality of <33%. In patients with SIRS the APACHE II score was 7, corresponding to 6% risk of death (Table 1).
SS was caused by Gram-negative pathogens in 63/117 (54%) of patients and in Gram-negative sepsis, E. coli (28/63; 44.4%) was the most frequent isolate. Gram-positive SS was present in 24/117 (20.5%) of cases and the most frequent pathogen was S. aureus (14/24; 58.3%), whereas C. albicans was the most frequent isolate in yeast-positive cultures (10/117; 8.5%) and blood cultures were polymicrobial in 20/117 (17%) cases. Bacterial isolates from positive blood culture are reported in Table 2.
PCT and MR-proADM in patients with SS and SIRS
Median values, interquartile ranges (25th percentile and 75th percentile) and Mann–Whitney comparison of PCT and MR-proADM analysed in patients with SS and SIRS are reported in Table 3. PCT and MR-proADM values were significantly higher in patients with SS than SIRS (P<0.0001) (Table 3 and Figure 1).
ROC curve and AUC analysis of PCT and MR-proADM in patients with SS
In SS patients, the area under curve (AUC) values of PCT and MR-proADM are reported in Table 4. Based upon ROC curve analysis and AUC characteristics, PCT and MR-proADM were considered applicable for sepsis diagnosis at the cut-off values of 0.5 ng/mL and 1 nmol/L, respectively (Table 4 and Figure 2).
Multiple logistic regression analysis
Multiple logistic regression analysis using SS as the dependent variable and PCT and MR-proADM as independent variables is reported in Table 5. Patients with MR-proADM >1 nmol/L have ~195 times the probability of being affected by SS than patients with SIRS, and patients with PCT values >0.5 ng/mL have the probability of developing SS 49 times more than SIRS.
Combined PCT and MR-proADM measurement in SS diagnosis: post-test probability calculation
In patients with SS, PCT and MR-proADM used as single markers have a post-test probability of 0.964 and 0.936, respectively. The combination of PCT and MR-proADM resulted in a higher value of post-test probability, 0.996 (Table 4).
Discussion
The early diagnosis and stratification of the severity of sepsis are essential, increasing the possibility of starting timely the specific treatment, especially in patients affected by SS. In this study, the combined measurement of PCT and MR-proADM in patients with SS was evaluated in order to establish the advantage derived from the use of a multimarker rather than a single marker approach.
PCT has been described as a reliable marker in the early diagnosis of sepsis compared to other plasma biomarkers or clinical data alone [13, 14, 19]. MR-proADM has been used as marker of disease severity in different clinical setting and recently its combination with PCT in bacterial infections and sepsis has been evaluated [28–32, 14, 19]. The combination of PCT and MR-proADM could allow the simultaneous evaluation of the presence of a bacterial infection as well as of the severity of this infection, giving to the ward clinicians a first useful indication waiting for blood culture positivity.
Results from this study demonstrated that in patients with SS, PCT and MR-proADM values are significantly higher than patients with SIRS. ROC curve analysis of PCT and MR-proADM demonstrated a high diagnostic accuracy of these two markers in SS diagnosis at the cut-off value of 0.5 ng/mL and 1 nmol/L, respectively. The logistic regression analysis showed higher OR values for both markers indicating a significant increased risk of having SS when these markers are higher than the cut-off values established. Furthermore, the combination of the two markers leads to a very high post-test probability value of about 99.6%.
These data confirmed the important role of the combination of PCT and MR-proADM in the diagnosis and prognosis of patients with sepsis rather than the single marker approach, because it combines the diagnostic ability of PCT with the prognostic value of MR-proADM, as already described in localized bacterial infections and not complicated sepsis [14, 19].
In conclusion, this study further support the advantage derived from the multi-marker approach in sepsis diagnosis and prognosis, especially in critically ill patients.
References
1. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013; 39: 165–228.
2. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 2003; 31: 1250–1256.
3. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001; 29: 1303–1310.
4. American College of Chest Physicians/Society of Critical Care Medicine. American College of Chest Physicians/Society of Critical Care Medicine consensus conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992; 20: 864–874.
5. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348: 1546–1554.
6. Russell JA. Management of sepsis. N Engl J Med. 2006; 355: 1699–1713.
7. Cherkaoui A, Hibbs J, Emonet S, Tangomo M, Girard M, et al. Comparison of two matrix-assisted laser desorption ionization time of flight mass spectrometry methods with conventional phenotypic identification for routine identification of bacteria to the species level. J Clin Microbiol. 2010; 48: 1169–1175.
8. Gullo A, Bianco N, Berlot G. Management of severe sepsis and septic shock: challenges and recommendations. Crit Care Clin. 2006; 22: 489–501.
9. Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001; 69: 89–95.
10. Marshall JC, Reinhart K. Biomarkers of sepsis. Crit Care Med. 2009, 37: 2290–2298.
11. Nakamura A, Wada H, Ikejiri M, Hatada T, Sakurai H, et al. Efficacy of procalcitonin in the early diagnosis of bacterial infections in a critical care unit. Shock 2009, 31: 591.
12. Vänskä M, Koivula I, Jantunen E, Hämäläinen S, Purhonen AK, et al. IL-10 combined with procalcitonin improves early prediction of complications of febrile neutropenia in hematological patients. Cytokine 2012; 60: 787–792.
13. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993; 341: 515–518.
14. Angeletti S, Spoto S, Fogolari M, Cortigiani M, Fioravanti M, et al. Diagnostic and prognostic role of procalcitonin (PCT) and MR-pro-Adrenomedullin (MR-proADM) in bacterial infections. APMIS 2015; 123: 740–748.
15. Kojic D, Siegler BH, Uhle F, Lichtenstern C1, Nawroth PP, et al. Are there new approaches for diagnosis, therapy guidance and outcome prediction of sepsis? World J Exp Med. 2015; 5: 50–63.
16. Hirata Y, Mitaka C, Sato K, Nagura T, Tsunoda Y, et al. Increased circulating adrenomedullin, a novel vasodilatory peptide, in sepsis. J Clin Endocrinol Metab. 1996; 81: 1449–1153.
17. Kitamura K, Kangawa K, Kawamoto M, Ichiki Y, Nakamura S, et al. Adrenomedullin: a novel hypotensive peptide isolated from human pheochromocytoma. Biochem Biophys Res Commun. 2012; 425: 548–555.
18. Zhou M, Ba ZF, Chaudry IH, Wang P. Adrenomedullin binding protein-1 modulates vascular responsiveness to adrenomedullin in late sepsis. Am J Physiol Regul Integr Comp Physiol. 2002; 283: R553–560.
19. Angeletti S, Battistoni F, Fioravanti M, Bernardini S, Dicuonzo G. Procalcitonin and mid-regional pro-adrenomedullin test combination in sepsis diagnosis. Clin Chem Lab Med. 2013; 51: 1059–1067.
20. Suberviola B, Castellanos-Ortega A, Ruiz Ruiz A, Lopez-Hoyos M, Santibañez M. Hospital mortality prognostication in sepsis using the new biomarkers suPAR and proADM in a single determination on ICU admission. Intensive Care Med. 2013; 39: 1945–1952.
21. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system Crit Care Med. 1985; 13: 818–829.
22. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998; 26: 1793–1800.
23. Kajdacsy-Balla Amaral AC, Andrade FM, Moreno R, Artigas A, Cantraine F, Vincent JL. Use of the sequential organ failure assessment score as a severity score. Intensive Care Med. 2005; 31: 243–249.
24. Angeletti S, Dicuonzo G, D’Agostino A, Avola A, Crea F. Turnaround time of positive blood cultures after the introduction of matrix-assisted laser desorption-ionization time-of-flight mass spectrometry. New Microbiol. 2015; 38: 379–386.
25. Christ-Crain M, Morgenthaler NG, Struck J, Harbarth S, Bergmann A, Müller B. Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care 2005; 9: R816–824.
26. Florkowski CM. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: communicating the performance of diagnostic tests. Clin Biochem Rev. 2008;29(Suppl 1): S83–7.
27. Albert A. On the use and computation of Likelihood ratios in clinical chemistry. Clin Chem. 1982; 28: 1113–1119.
28. Maisel A, Mueller C, Nowak R, Peacock WF, Landsberg JW, et al. Mid-Region pro-hormone markers for diagnosis and prognosis in acute dyspnea. J Am Coll Cardiol. 2010; 55: 2062–2076.
29. Maisel A, Mueller C, Nowak R, Peacock WF, Ponikowski P, et al. MidRegion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea. J Am Coll Cardiol. 2011; 58: 10572–10567.
30. Paecock WF, Nowak R, Christenson R, DiSomma S, Neath SX, et al. Short-term mortality risk in emergency department acute heart failure. Acad Emerg Med. 2011; 18: 947–958.
31. Travaglino F, De Berardinis B, Magrini L, Bongiovanni C, Candelli M, et al. Utility of procalictonin (PCT) and mid regional pro-adrenomedullin (MR-proADM) in risk stratification of critically ill febrile patients in emergency department (ED). A comparison with APACHE II score. BMC Infect Dis. 2012; 12: 184.
32. Hagag AA, Elmahdy HS, Ezzat AA. Prognostic value of plasma pro-adrenomedullin and antithrombin levels in neonatal sepsis. Indian Pediatr. 2011; 48: 471–473.
The authors
S. Angeletti*1 MD, M. De Cesaris1, A. Lo Presti2 PhD, M. Fioravanti1, F. Antonelli1, R. Ottaviani1, L. Pedicino1, A. Conti1, A. M. Lanotte1, M. Fogolari1 MD, M. Ciccozzi2 PhD, G. Dicuonzo1 MD
1Clinical Pathology and Microbiology Laboratory, University Hospital Campus Bio-Medico of Rome, Italy
2Department of Infectious, Parasitic, and Immune-Mediated Diseases, Epidemiology Unit, Reference Centre on Phylogeny, Molecular Epidemiology, and Microbial Evolution (FEMEM), National Institute of Health, Rome, Italy
*Corresponding author
E-mail: s.angeletti@unicampus.it