During the course of the current coronavirus pandemic we have all been aware of the urgent need for nucleic acid testing to identify people currently infected with SARS-CoV-2. The second test that is needed, the serology test, to identify who has had the virus, is much more complex to produce. Dr Andy Lane, commercial director from The Native Antigen Company, discusses adaptive immunity and the production of antigens and antibodies for the creation of immunoassays that can be used for in vitro diagnostics.
What is The Native Antigen Company and what does it do?
The Native Antigen Company was founded in Oxford, UK, in 2010, with the goal of developing native viral and bacterial antigens to support the in vitro diagnostics (IVD) industry. The company was the first to release highly pure Zika virus NS1 antigens for the development of specific diagnostics in 2016, and has since built experience and capabilities to support the research community in pandemic scenarios. In February 2020, the company became one of the firstrecognized suppliers of antigens for SARS-CoV-2 (the virus that causes COVID-19), and has continued to develop a broad and expanding range of coronavirus reagents. Additionally, we offer a wide variety of native and recombinant antigens for over 60 infectious diseases and provide custom and contract services to the life sciences and biotechnology industries.
Our reagents are used by a wide range of researchers working in infectious diseases, but are predominantly sold into two major markets: the IVD industry, who use antigens and antibodies to develop immunoassays for serological diagnosis of infection, and the vaccine industry, who use antigens and antibodies to develop immunoassays for the qualification and quantification of animal and patient vaccine responses in clinical trials.
Briefly, how is immunity generated in response to infection?
It goes without saying that the human immune system is highly complex, but it can generally be broken down into the innate and adaptive immune responses. Innate immunity is our first line of defence. It provides a rapid, but somewhat makeshift response that is largely preoccupied with trying to kill infectious agents from the moment they enter the body, with a broad array of non-specific cells, proteins and biochemicals. While this is ongoing, the innate response alerts the adaptive response. Adaptive immunity (overview in Fig. 1) represents the elite troops of the immune system, which launch an attack that is specifically adapted to the infectious agent using more sophisticated weapons to mediate powerful downstream responses. The hallmark of the adaptive response is clonal expansion, where B and T lymphocytes that are able to recognize a pathogen will be positively selected for to rapidly build their numbers. Once these cells reach significant levels, the body is much better equipped to detect and clear the invading pathogen, and tends to form a long-lasting ‘memory’ of the pathogen to better prepare itself for future encounters.
After some viral infections, we develop lifelong immunity; however, after others we are only protected for a short period of time – why does this difference arise?
There are two major reasons for reinfection by a virus shortly after initial exposure. The first is due to the ability of viruses to mutate, which occurs via the natural accumulation of genetic changes over time (antigenic drift) or recombination of a virus’s genome with a related strain, causing it to rapidly mutate into a novel form (antigenic shift). These processes allow a virus to change its ‘appearance’, such that it is no longer recognizable by our immune system, and makes our previous exposure to the original virus of little use. This is best exemplified by the influenza A virus, which is notorious for mutating its surface proteins (hemagglutinins and neuraminidases) to evade immune recognition, resulting in a perpetual game of cat and mouse that requires the development of new vaccine formulations every flu season.
The second reason for ineffective immune responses is a bit more complex and tends to occur as a result of waning memory cell levels in the host’s immune system following initial infection. However, the cause of short-lived immunity is not entirely clear and largely depends on the virus in question as well as myriad influencing factors, such as genetics, age and previous exposure to pathogens. A very relevant example are the endemic coronaviruses, such as OC43-CoV and 229E-CoV, whose infections may result in only a few months of immunity. A study in the early 90s, for example, showed that exposure with 229E-CoV only one year after initial infection resulted in reinfection in the majority of patients and correlated with declining antibody titres [1]. The reason for the decline in immune memory is not entirely clear but is often attributed to the mild pathogenicity of such viruses eliciting a somewhat lacklustre immune response in the first place.
Given the short-lived immunity of some coronaviruses, COVID-19 immunity has been a hot topic. Most patients have shown quite potent and lasting antibody responses, while some have little-to-no detectable antibodies following infection [2]. While we are not yet sure whether this is an immune phenomenon or an issue of poor assay sensitivity, it will take some time before we are able to truly understand the human body’s response to this disease.
Serology testing is of great importance in clinical diagnostics. When doing serology testing to see if a person has had a disease, what exactly is being detected and how is this usually achieved?
By definition, serology is the scientific examination of blood serum and its components. However, in the context of the clinical diagnosis of infectious disease, it generally refers to the use of immunoassays that measure antigens or antibodies. Immunoassays are found in a wide variety of formats but are best exemplified by the enzyme-linked immunosorbent assay (ELISA), which uses plastic titer plates to bind antigens or antibodies from patient samples and produce a detectable signal.
The second major immunoassay format is the lateral flow assay (LFA), which uses an absorbent pad to absorb an analyte and run it through a series of specific antibodies to produce a detectable signal. These assays have the advantage of being inexpensive and portable and can typically provide results within minutes.
Emerging studies suggest that the serology of SARS-CoV-2 is highly complex and differs significantly from other betacoronaviruses. Antibody responses to SARS-CoV-2 appear to occur later and be of lower titres than are typically observed for viral infections, influencing the way in which assays are designed to diagnose both acute and historic infections. Another important consideration is the potential for antibody cross-reactivity to other co-circulating coronaviruses, requiring close attention to the binding specificity of antigens used.
In the current COVID-19 pandemic, serology testing will be crucial for discovering much about the disease – what will we be hoping to learn from this?
From the outset of the pandemic, the reverse-transcriptase polymerase chain reaction (RT-PCR) has been the predominant means of diagnosing active infection. However, as molecular methods rely on the presence of viral nucleic acids, they are limited to a narrow window during the acute phase of infection when the virus is present in the respiratory tract. This has left a major gap in the ability to detect previous cases and understanding the transmission dynamics of this disease. Antibodies to SARS-CoV-2, however, may last for some time after infection to allow for retrospective diagnosis once patients have recovered. This is particularly useful for multiple reasons.
First, as governments ease lockdown restrictions, high-quality epidemiological data is vital for keeping an eye on temporal and geographical disease dynamics, which will require frequent sampling of antibodies in populations (serosurveys). There is also a clear advantage in using serology tests for diagnosis at the point of care. Unlike high-throughput RT-PCR or ELISAs, LFAs present a highly practical and rapid alternative for acute-phase diagnosis and will be crucial in identifying asymptomatic carriers and infected individuals to ensure they are isolated from the general population.
Another major role of serology is in vaccine testing. So far, there are over 130 vaccine candidates currently in the pipeline [3]. While these vaccines are based on a wide range of platforms, (including mRNA, DNA, nanoparticles, subunits, synthetic peptides and virus-like particles, to name a few), it can be said with near certainty, that a SARS-CoV-2 vaccine will elicit immune responses to the spike protein. However, considering that vaccine-induced anti-spike IgG levels may be indistinguishable from those conferred by natural infection, alternative antigens will be needed to design vaccine-specific assays. These assays will also be very useful in assessing the potential risk of vaccine-induced antibody-dependent enhancement, in which antibodies produced by a vaccine are able to facilitate a more aggressive pathogenesis when a patient gets a real SARS-CoV-2 infection.
How do you go about preparing reagents for a serology test for a new pathogen such as SARSCoV- 2 and why is it important that these reagents are ‘native-like’?
When developing any immunoassay, the most important components are the antigens and antibodies used to design it. The considerations for choosing these reagents are wide-ranging: antigens should include the most appropriate epitopes to facilitate high sensitivity and antibodies should be tested for high affinity to the antigen in question. When considering specificity, it is crucial to ensure than detector antibodies do not bind to the cross-reactive epitopes that are often found on more conserved regions of viral antigens.
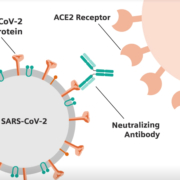
To modulate the sensitivity and specificity of an assay, specific portions of a protein can also be used. In the case of SARS-CoV-2, researchers are investigating various different regions of its spike protein for use in immunoassays. The S1 and S2 subunits of the spike are a popular choice for the development of immunoassays as they are highly exposed to the virus’s external environment and can readily induce potent antibody responses. In particular, anti-spike antibodies that bind the receptor-binding domain (RBD) of S1 may be able to neutralize virus by preventing binding with ACE2. The spike RBD functions to mediate cell-surface attachment and internalization by binding human ACE2 receptors. Given RBD’s role in host-cell entry, it is able to elicit highly neutralizing antibody responses and is a popular target for the development of vaccines. The RBD also shows high sequence divergence between other coronavirus spike proteins, making it a popular antigen for the development of sensitive and specific immunoassays. The N-terminal domain of the SARS-CoV-2 spike protein shows the highest sequence variability across the coronavirus family, making it a popular choice of antigen for maximizing the specificity of diagnostic assays.
Given the biosafety implications of handling a live virus, recombinant antigens expressed from other organisms are the go-to for developing assays. However, not all expression systems are born equal. Simple organisms like Escherichia coli are easy to genetically manipulate but lack the necessary post-translational machinery to glycosylate proteins. Incidentally, each SARS-CoV-2 spike trimer contains up to 66 glycan sugars to facilitate folding and mediate viral tropisms, amongst other things. From the perspective of assay development, these glycans constitute many of the key surface epitopes that are recognized by detector antibodies and the use of unglycosylated spike risks the binding of non-specific, cross-reacting antibodies that can reduce diagnostic specificity.
To ensure that spike is produced with its full glycosylation pattern and is properly folded, more complex systems need to be used. At The Native Antigen Company, we use our VirtuE mammalian (HEK293) system that has been developed for the bespoke purpose of expressing high-quality antigens with proper folding and full glycosylation.
What’s your vision for the future for The Native Antigen Company and its collaboration with OXGENE?
After the SARS-CoV-2 genome was published in early January, it was an all-out race to develop and release reagents. After a tremendous effort by our R&D team, we managed to produce our first batch of S1 antigens in early February and began to ship them to our customers around the globe. However, the next challenge was manufacturing capacity. Given the demand from the IVD and vaccine industries, we soon began to struggle in meeting such large demand. Fortunately, we were able to reach out to some manufacturers who could support us with scale production.
Our first partner, OXGENE™ has been using their Protein Machine Technology to develop stable cell lines for the production of spike antigens. Their technology uses a proprietary adenoviral vector to carry SARS-CoV-2 DNA into human cells, where it delivers it to the nucleus for stable integration. From here, cell lines can be cultured en masse to produce large quantities of protein without the inherent limitations in yield of transient expression. Work is still ongoing to optimize expression, but we’re hoping for some positive data in the coming weeks.