Heart fatty acid binding protein and troponin: a match made in heaven?
Plasma levels of heart-type fatty acid binding protein (H-FABP) have been shown to rise early after the onset of acute myocardial infarction (AMI). Recent evidence suggests combining H-FABP with troponin gives superior diagnostic accuracy compared to the alternative ‘early markers’ of myocardial necrosis, creatine kinase-MB (CK-MB) and myoglobin. However, using a single measurement at the time of presentation to the Emergency Department (ED), H-FABP is unlikely to have sufficient sensitivity to safely ‘rule out’ AMI, even when combined with a standard troponin assay. With the advent of high sensitivity troponin assays which have higher diagnostic sensitivity at the time of presentation, it is possible that H-FABP could be combined with levels of high sensitivity troponin and potentially with other clinical information to enable safe ‘rule out’ of AMI using a single blood test at the time of presentation. Further work in this area is needed.
by Dr Richard Body
Background
Suspected cardiac chest pain accounts for approximately one quarter of acute medical admissions, although only a minority of the patients admitted will ultimately be diagnosed with an acute coronary syndrome [1]. Meanwhile, up to 2% of patients with acute myocardial infarction (AMI) have that diagnosis missed and are inadvertently discharged, leading to a worse prognosis [2]. There is therefore tremendous potential to reduce unnecessary hospital admissions in this patient group, although advances in diagnostic technology are clearly necessary in order to do so.
High sensitivity troponin
Cardiac troponins are regulatory proteins contained within the myofibrillar apparatus of cardiac myocytes. They are released into the bloodstream following myocardial necrosis and their detection allows highly sensitive and specific diagnosis of AMI. Indeed, the detection of a rise and/or fall of cardiac troponin in serum or plasma is integral to the diagnosis of AMI. With the advent of high sensitivity troponin (hs-cTn) assays, which have greater analytical and diagnostic sensitivity than standard assays, it is tempting to believe that the hunt for an ‘early rule out’ strategy for acute coronary syndromes is over. Standard troponin assays lack the diagnostic sensitivity to enable safe exclusion of acute myocardial infarction (AMI) when measured at the time of presentation. This creates a period of ‘troponin blindness’, when patients with AMI still have low circulating troponin levels prior to the development of a late troponin rise. Hs-cTn assays have been shown to improve diagnostic sensitivity at the time of initial presentation to the Emergency Department (ED). While this reduces the magnitude of our problem with ‘troponin blindness’, it does not overcome the problem completely. Even hs-cTn assays fail to identify approximately 10% of patients with AMI at the time of presentation [3, 4]. With hs-cTn assays it may be possible to reduce the time taken to confidently ‘rule out’ AMI with serial sampling from 6 to 9 hours after arrival (or 10–12 hours from symptom onset) to as little as 3 hours after arrival [4, 5]. This approach still needs to be validated against a hs-cTn reference standard, however, and there are a few other reasons to be cautious. The sensitivity of the Siemens troponin I Ultra assay (a sensitive assay but not high sensitivity), which had a diagnostic sensitivity of 100% at 3 hours after presentation in Keller et al.’s original study (evaluated against the reference standard of testing 6 hours after arrival), was actually only 94.5% at 6 to 12 hours from symptom onset [4]. Further, high sensitivity troponin T (hs-cTnT) has been shown to have a sensitivity of only 92.2% when measured 2 hours after presentation, which is still some way from a satisfactory rule out strategy [6]. Using the new Abbott Architect high sensitivity troponin I assay, sensitivity for AMI is 98.2% (with 95% confidence intervals extending down to 96.9%), again using a standard troponin assay as the reference standard [5]. Even if we accept that no rule out strategy will be 100% sensitive and consider this 3-hour troponin to be a satisfactory rule out strategy, that still means an anxious wait for patients and would still, in health systems like the United Kingdom, necessitate admission to an inpatient ward for investigation.
Interest in ‘early markers’ of myocardial necrosis
There has been interest in the role of ‘early markers’ of myocardial necrosis for many years. As troponin is predominantly an intracellular constituent and levels do not peak for 12 to 24 hours after the onset of infarction [7], many have investigated the value of biomarkers with release kinetics suggesting that they may enable earlier identification of AMI. Thus, the measurement of creatine kinase-MB (CK-MB) and myoglobin levels in combination with troponin were shown to improve early diagnosis of AMI as early as 2001 [8]. More recently, the ASPECT study from 14 countries in the Asia-Pacific region examined the value of CK-MB, myoglobin and troponin I (using assays from Alere, San Diego, CA, USA) measured at presentation and 120 minutes later in patients with a Thrombolysis In Myocardial Infarction (TIMI) score of 0/7. The authors found that 9.8% of patients could be discharged using this strategy with a 0.9% incidence of adverse cardiac events within 30 days [9]. Around the same time, the Randomised Assessment Using Panel Assay of Cardiac Biomarkers (RATPAC) study demonstrated that serial evaluation of CK-MB, myoglobin and troponin I over 90 minutes led to an increase in the proportion of patients successfully discharged from the ED, although this came at a cost of rebound-overuse of Coronary Care resources, perhaps as a function of the lack of specificity of myoglobin and CK-MB. The strategy was found to be not cost effective [10].
Heart-type fatty acid binding protein
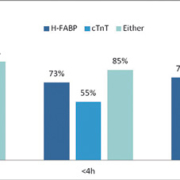
Heart-type fatty acid-binding protein (H-FABP) is a cytosolic protein that is abundantly expressed in human myocardial cells, where it facilitates intracellular fatty acid transport within cardiac myocytes [11]. Plasma H-FABP levels rise early after the onset of AMI. McCann et al. evaluated H-FABP (Hycult Biotechnology ELISA) and troponin T (cTnT; Roche Elecsys, 4th generation) in 415 patients who were admitted to an acute cardiology unit on suspicion of an acute coronary syndrome. They demonstrated that H-FABP had superior sensitivity to troponin in patients who presented early (<4h) after symptom onset [Figure 1] [12]. A meta-analysis of 16 studies including 3,709 patients with suspected AMI demonstrated a pooled sensitivity of 84% [95% confidence intervals (CI) 76–90%] and a pooled specificity of 84% (95% CI 76–89%), although there was significant heterogeneity between studies [13]. It is clear that measurement of H-FABP alone cannot enable safe ‘rule out’ of AMI.
Combining H-FABP with troponin will, however, yield a higher diagnostic sensitivity. Body et al. [14] demonstrated that the combination of H-FABP and troponin I offers both superior sensitivity and superior specificity to the combination of CK-MB, myoglobin and troponin I [Figure 2].
A systematic review by Carroll et al. demonstrated that, in 4 studies, the combination of H-FABP and troponin had an overall sensitivity of between 76 and 97% [15]. Two of these studies did, however, use insensitive troponin assays with diagnostic sensitivities of 42% and 55% respectively. The use of more sensitive troponin assays may be expected to yield higher diagnostic performance. Indeed, in the study by Body et al., the sensitivity of the combination of H-FABP and troponin increased from 82% to 87% when a more sensitive troponin assay was used [14, 16]. If only low risk patients (using the modified Goldman risk stratification tool) who had normal H-FABP and normal cTnT were considered for early discharge, a sensitivity and negative predictive value of 99% could be achieved, although this strategy may have a specificity as low as 19%, meaning that only a minority of patients would be eligible for early discharge while 1% of AMIs would still be missed [16].
H-FABP and high sensitivity troponin
It is clear that neither H-FABP nor troponin (even using a high sensitivity assay) can be used to safely exclude a diagnosis of AMI when measured at the time of presentation to the ED. The combination of H-FABP and standard troponin assays improves overall diagnostic sensitivity but is still unable to ‘rule out’ this important diagnosis. By combining H-FABP with high sensitivity troponin assays, it may be possible to further increase sensitivity and thus achieve an effective early rule out strategy. Evidence in this area is still limited. However, Aldous et al. did evaluate the combination of H-FABP (Hycult Biotech) and hs-cTnT in a cohort of 384 patients presenting to the ED with suspected acute coronary syndromes. This combination had a sensitivity of 90.0% for AMI and a specificity of 73.5%. Notably, the sensitivity of the H-FABP assay alone was particularly low in this study (50.0%), which may be a function of the high diagnostic cut-off employed (60ng/ml) when compared to the cut-off employed by McCann et al. using the same assay (5ng/ml) [12, 17]. Using this high diagnostic cut-off, however, the combination of H-FABP and hs-cTnT measured at the time of presentation may help to ‘rule in’ the diagnosis of AMI, with a specificity of 99.4% (95% CI 97.9–99.9%) [17].
Inoue et al. also evaluated both hs-cTnT and H-FABP (DS Pharma Biomedical, Osaka) in 432 ED patients with suspected acute coronary syndromes. In this study, H-FABP had a similar area under the receiver operating characteristic (ROC) curve (AUC) to hs-cTnT (0.83 versus 0.82), although hs-cTnT had a higher sensitivity at the diagnostic cut-off (87.9% vs. 78.5%) [18]. The authors do not report the diagnostic value of the combination of both biomarkers. Meanwhile, in 1,818 patients with suspected acute coronary syndromes, Keller et al. reported that H-FABP had an AUC of 0.89, which rose to 0.97 when combined with high sensitivity troponin I (Abbott Architect STAT high sensitive troponin) [5]. This implies that the combination has high diagnostic accuracy, although the sensitivity and negative predictive value of the strategy were not reported.
H-FABP and prognosis
H-FABP levels may also have prognostic value in patients with suspected acute coronary syndromes. Viswanathan et al. studied 1,080 consecutive patients presenting with suspected acute coronary syndromes [19]. They measured both H-FABP (Randox Evidence Biochip) and troponin I using a sensitive assay (Siemens Advia troponin I Ultra) and followed patients for a median of 18 months. H-FABP predicted death or AMI occurring during follow up, even in troponin negative patients and after adjustment for age and serum creatinine. For predicting death or AMI, H-FABP had an AUC of 0.79 (95% CI 0.74–0.84)
compared to 0.77 (95% CI 0.72–0.82) for troponin I.
Future work
Further work is still needed to determine whether the combination of H-FABP and high sensitivity troponin will enable safe rule out of acute coronary syndromes in the ED. Combination with other clinical information available from risk stratification tools (such as the modified Goldman or TIMI scores) or the ECG may further increase sensitivity, enabling AMI to be safely excluded in a proportion of patients presenting to the ED. Further, with the increase in false positive results given by high sensitivity troponin assays, H-FABP may help to ‘rule in’ the diagnosis of AMI in patients with troponin elevations at the time of presentation, before the results of serial testing are available. This will facilitate early treatment and triage to an appropriate level of care in the hospital, while avoiding the risks of unnecessary treatment for those patients with false positive elevations.
Conclusions
H-FABP is a promising biomarker for use in patients with suspected acute coronary syndromes. Used alone or in combination with a standard troponin assay, sensitivity will be insufficient to safely ‘rule out’ AMI. Further work is needed to determine whether combination with a high sensitivity assay can enable safe ‘rule out’ for a proportion of patients, and to evaluate whether H-FABP may have a role in the differentiation between ‘true positive’ and ‘false positive’ troponin elevations at the time of initial presentation.
References
1. Goodacre S, et al. The health care burden of acute chest pain. Heart 2005; 91: 229–230.
2. Pope JH, et al. Missed diagnoses of acute cardiac ischaemia in the Emergency Department. N Engl J Med 2000; 342: 1163–1170.
3. Reichlin T, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009; 361: 858–867.
4. Keller T, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med 2009; 361(9): 868–877.
5. Keller T, et al. Serial changes in highly sensitive troonin I assay and early diagnosis of myocardial infarction. JAMA 2011; 306(24): 2684–2693.
6. Aldous SJ, et al. Diagnostic and prognostic utility of early measurement with high-sensitivity troponin T assay in patients presenting with chest pain. CMAJ 2012; 184: E260-E268.
7. Tucker JF, et al. Early diagnostic efficiency of cardiac troponin I and troponin T for acute myocardial infarction. Acad Emerg Med 1997; 4(1): 13–21.
8. McCord J, et al. Ninety-minute exclusion of acute myocardial infarcdtion by use of quantitative point-of-care testing of myoglobin and troponin I. Circulation 2001; 104: 1483–1488.
9. Than M, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet 2011; 377(9771): 1077–1084.
10. Fitzgerald P, et al, on behalf of the RATPAC investigators. Cost-effectiveness of point-of-care biomarker assessment for suspected myocardial infarction: The RATPAC trial (Randomised Assessment of Treatment Using Panel Assay of Cardiac markers). Acad Emerg Med 2011; 18(5): 488–495.
11. Schaap FG, et al. Impaired Long-Chain Fatty Acid Utilization by Cardiac Myocytes Isolated From Mice Lacking the Heart-Type Fatty Acid Binding Protein Gene. Circ Res 1999; 85(4): 329–337.
12. McCann C, et al. Novel biomarkers in early diagnosis of acute myocardial infarction compared with cardiac troponin T. Eur Heart J 2008; 29(23): 2843–2850.
13. Bruins Slot MH, et al. Heart-type fatty acid-binding protein in the early diagnosis of acute myocardial infarction: a systematic review and meta-analysis. Heart 2010; 96(24): 1957–1963.
14. Body R, et al. A FABP-ulous ‘rule out’ strategy? Heart fatty acid binding protein and troponin for rapid exclusion of acute myocardial infarction. Resuscitation 2011; 82(8): 1041–1046.
15. Carroll C, et al. Heart-type fatty acid binding protein as an early marker for myocardial infarction: systematic review and meta-analysis. Emerg Med J 2012.
16. Body R, et al. Reply to Letter: Still FABP-ulous even with a more sensitive troponin assay. Resuscitation 2012; 83(2): e29–e30.
17. Aldous S, et al. Heart fatty acid binding protein and myoglobin do not improve early rule out of acute myocardial infarction when highly sensitive troponin assays are used. Resuscitation 2012; 83(2): e27–e28.
18. Inoue K, et al. Heart fatty acid-binding protein offers similar diagnostic performance to high-sensitivity troponin T in Emergency Room patients presenting with chest pain. Circulation 2011; 75: 2813–2820.
19. Viswanathan K, et al. Heart-Type Fatty Acid-Binding Protein Predicts Long-Term Mortality and Re-Infarction in Consecutive Patients With Suspected Acute Coronary Syndrome Who Are Troponin-Negative. J Am Coll Cardiol 2010; 55(23): 2590–2598.
The author
Richard Body, MB ChB MRCSEd(A&E) FCEM PhD
Emergency Department,
Manchester Royal Infirmary,
Oxford Road, Manchester, M13 9WL, UK
e-mail: richard.body@manchester.ac.uk