Intraductal tubulopapillary neoplasm of the pancreas
Intraductal tubulopapillary neoplasm is a recently recognized distinct and rare entity of the pancreas, which may be unfamiliar to many physicians and laboratory personnel. However, recognizing this disease is critical for its proper clinical management and further study. Here, we discuss the clinical and pathological features of this neoplasm.
by Dr Shula Schechter and Dr Jiaqi Shi
Presentation and definition of intraductal tubulopapillary neoplasm of the pancreas
Intraductal tubulopapillary neoplasm (ITPN) was recently recognized as a distinct neoplastic entity of the pancreas in the 2010 edition of the World Health Organization (WHO) classification [1]. It was defined as an intraductal, grossly visible, tubule-forming epithelial neoplasm with high-grade dysplasia and ductal differentiation without overt production of mucin, although focal tubulopapillary growth is also acceptable [1].
ITPN is a rare entity. Although it was first described in the mid-1990s by Japanese investigators and has been termed ITPN since 2009 [2], its diagnostic criteria need to be refined and recognition of this disease needs to be improved. The differential diagnosis of ITPN can be complex because its features overlap with other more common intraductal neoplasms, such as intraductal papillary mucinous neoplasm (IPMN). A recently published literature review and a large study of 33 cases of ITPN have shed some light on the clinicopathologic and immunohistochemical features of this disease and further advance our knowledge of its diagnosis [3, 4].
The majority of the patients with ITPN present with abdominal pain, nausea, vomiting, weight loss and steatorrhea. A few patients have diabetes mellitus, acute pancreatitis, jaundice and fever. Incidental discovery of ITPN occurs in about one-third of patients. The risk factors for ITPN are not well defined, but there are reports of an association of ITPN with radiation exposure and with a family history of pancreatic cancer [4–6]. The incidence of ITPN in men and in women is comparable. Most ITPNs occur in the sixth decade with a range in age of 25 to 79 years. Nearly half of reported ITPNs are located in the head of the pancreas. In the remainder of cases, the location of the ITPN is divided between the body and tail with about one-quarter of lesions showing more extensive involvement of the entire pancreas [4]. ITPNs are often slow growing tumours and large at the time of discovery.
Imaging studies with dynamic contrast-enhanced computed tomography and magnetic resonance imaging are commonly used to assist with preoperative diagnosis. A helpful imaging clue for the diagnosis of ITPN is the two-tone duct sign, which is a reflection of tumour in the main pancreatic duct with ductal dilation upstream [7]. With magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography, ITPN also has a characteristic finding, the so called ‘cork-of-wine-bottle’ sign, which results from intraductal growth of the tumour [7].
Information on the prognosis of ITPNs is limited by the small number of reported cases, although data have suggested an excellent prognosis for patients without invasion (overall 5-year survival rate of 100%) and a significantly more favourable prognosis for ITPNs with a component of invasive carcinoma (overall 5-year survival rate of 71%) relative to the traditional invasive pancreatic ductal adenocarcinoma (overall 5-year survival rate <10%) [2, 8, 9]. However, the extent of invasion does not necessarily correlate with clinical outcome. Patients with minimal invasion can die of disease, whereas patients with a large volume of invasion can achieve long-term survival [4]. Unfortunately, invasive carcinoma is present in most (54–71%) ITPNs and may be more likely in men [3, 4, 10]. In addition, tumours that are large in size, or have increased mitosis and a high Ki-67 proliferation index may have an increased association with invasive carcinoma [2]. Despite the favourable prognosis, the possibility of invasive carcinoma, recurrence and metastasis has led to the general recommendation of surgery as treatment in most ITPN patients.
Diagnostic features of ITPN based on histology and immunohistochemistry
Macroscopically, the mean size of the tumour is 3.8 cm (range 0.5–15 cm). Most ITPNs are circumscribed solid or polypoid masses obstructing pancreatic ducts. They generally arise in the main pancreatic duct, but approximately 5% arise within the branch ducts [4, 10]. ITPNs may be cystic, this occurs in less than half of cases. However, ITPNs do not have grossly identifiable mucin.
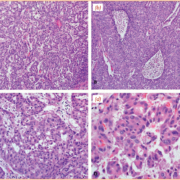
Microscopically, ITPNs are characterized by back-to-back tubules forming complex cribriform structures (Fig. 1a, c) with focal areas of papillary architecture seen in 36% of ITPN cases [4]. Solid growth with necrotic foci can occur, occasionally with areas of comedo-like necrosis (Fig. 1b). Occasionally, there are apical apocrine snouts and intraluminal secretion; however, cytoplasmic and intraluminal mucin is scant to absent. The tubules are lined by cuboidal to low columnar epithelial cells with minimal to moderate amounts of eosinophilic or amphiphilic cytoplasm and round to oval nuclei with moderate to marked atypia (Fig. 1d). ITPNs classically have uniform high-grade dysplasia and increased mitotic figures. Uncommon clear cell morphology or stromal osseous and cartilaginous metaplasia has also been reported in an ITPN.
By immunohistochemistry, all ITPNs to date have stained positively with anti-cytokeratin (CK) 7 (Table 1) and CAM5.2 antibodies. CK19 is positive in 92% of the cases. Tumour markers CA19.9 and CEA (carcinoembryonic antigen) are expressed in 93% and 50% of the cases respectively. In contrast, CK20 and CDX2 (homeobox protein CDX-2) only stain rare cells in a minority of ITPNs. The mucin (MUC) family has a particular staining pattern in ITPNs (Table 1), which is sometimes helpful in its differential diagnosis. MUC1 and MUC6 are positive in the majority of cases (88% and 77% respectively) whereas MUC2 and MUC5AC are usually negative (only 2% and 6% ITPNs are positive respectively). Nuclear p53 and p16-INK4 (cyclin-dependent kinase inhibitor 2A) are expressed in 27% and 33% of the cases. Rare focal or scattered cells can be positive for HepPar-1 antigen, chromogranin or nuclear β-catenin. However, ITPNs do not express pancreatic enzymes, trypsin and chymotrypsin, or loss of E-cadherin or Smad4.
Recent molecular findings
Recent genetic studies have found evidence that ITPN is molecularly distinct from IPMN. The most commonly mutated genes in ITPN include PIK3CA, TP53 and CDKN2A, among others [8–18]. Other rare mutations in histone H3 methyltransferase genes, MLL2 and MLL3 (also known as KMT2A and KMT2C), and MCL1 amplification have also been identified in ITPN [19]. However, ITPNs have been shown to have no or rare mutations in KRAS, BRAF, or GNAS. In contrast, IPMNs have high mutation rates in multiple genes [20]. KRAS mutation is thought to be one of the driver genes during IPMN development and mutations in GNAS and RNF43 are also common.
Differential diagnosis
Despite its distinct molecular features, the histology of ITPN can resemble that of IPMN, especially the pancreatobiliary and oncocytic type, making it difficult to distinguish ITPNs from IPMNs by morphology alone. The key morphologic features that characterize ITPNs as compared to IPMNs are shown in Table 2 and Figure 2. Overall, cystic components are infrequent with ITPNs in contrast to IPMNs, which are predominantly cystic lesions. Mucin is another distinguishing feature, which is sparse or absent with ITPNs but abundant with IPMNs. IPMNs also have significantly more morphologic variation according to epithelial subtype, and their degree of cytologic and architectural atypia varies from low- to high-grade dysplasia, whereas ITPNs typically demonstrate uniform high-grade dysplasia. On the other hand, comedo-like necrosis is frequent with ITPNs but rare with IPMNs.
The cytologic and architectural distinctions between ITPNs and IPMNs are confounded by the wide spectrum of morphologies and degree of dysplasia that are seen with IPMNs. Among the four recognized epithelial subtypes of IPMN, the pancreatobiliary and oncocytic type IPMN are the types that are most easily confused with ITPN. Similar to ITPN, both pancreatobiliary and oncocytic type IPMNs have high-grade dysplasia and often complex architecture. Nevertheless, the architecture of these IPMN subtypes remains predominantly papillary in nature as compared to the tubular or tubulopapillary architecture of ITPNs. In addition, the oncocytic IPMN has intraepithelial lumens as well as cells with abundant granular eosinophilic cytoplasm. Subtypes of IPMN also differ from ITPN in their immunohistochemical profiles. Most ITPNs are MUC6 positive and MUC5AC negative, whereas the opposite is true for most IPMNs (MUC6 negative and MUC5AC positive). The immunohistochemical findings with the oncocytic subtype of IPMN are most similar to findings with ITPNs, although some studies found MUC5AC can be positive with oncocytic IPMNs. Use of a mitochondrial stain (e.g. phosphotungstic acid–hematoxylin, Novelli stain, anti-apoptin 111.3 antibody) may allow an oncocytic IPMN to be distinguished from an ITPN on the basis of abundant mitochondria in cytoplasm [12].
Intraductal acinar cell carcinoma can also be confused with ITPN due to its occasional intraductal growth pattern. However, intraductal acinar cell carcinoma will typically stain positively for pancreatic enzymes such as trypsin, chymotrypsin or Bcl-10 (B-cell lymphoma/leukemia 10), and negatively for CK7 and CK19 by immunohistochemistry [4, 21].
Conclusion
ITPN is a relatively new diagnostic entity that occurs infrequently, predominantly in older patients. One-third of patients can be asymptomatic. Although invasive carcinoma is present in most ITPNs, the prognosis of these tumours appears to be significantly more favourable than pancreatic ductal adenocarcinoma. ITPNs generally arise in and obstruct the main pancreatic duct with circumscribed, solid nodules that are grossly visible. Histologically, these tumours are characterized by back-to-back tubules forming complex cribriform structures and uniform high-grade dysplasia. Necrosis is frequent but cytoplasmic and intraluminal mucin is scant to absent, which is in contrast with IPMNs. Molecular studies support that ITPN is a distinct entity from other intraductal neoplasms of pancreas, such as IPMN. With increased recognition of ITPNs, we expect to learn more information about its pathological features and prognostic implications.
References
1. Adsay NV, Fukushima N, Furukawa T, Hruban RH, Klimstra DS, Klöppel G, et al. Intraductal neoplasms of the pancreas. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, eds. World Health Organization Classification of Tumours of the Digestive System, pp. 304–313, 4th edn. International Agency for Research on Cancer 2010.
2. Yamaguchi H, Shimizu M, Ban S, Koyama I, Hatori T, Fujita I, Yamamoto M, Kawamura S, Kobayashi M et al. Intraductal tubulopapillary neoplasms of the pancreas distinct from pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol 2009; 33(8): 1164–1172.
3. Rooney SL, Shi J. Intraductal tubulopapillary neoplasm of the pancreas: an update from a pathologist’s perspective. Arch Pathol Lab Med 2016; 140(10): 1068–1073.
4. Basturk O, Adsay V, Askan G, Dhall D, Zamboni G, Shimizu M, Cymes K, Carneiro F, Balci S et al. Intraductal tubulopapillary neoplasm of the pancreas: A clinicopathologic and immunohistochemical analysis of 33 cases. Am J Surg Pathol 2017; 41(3): 313–325.
5. Bhuva N, Wasan H, Spalding D, Stamp G, Harrison M. Intraductal tubulopapillary neoplasm of the pancreas as a radiation induced malignancy. BMJ Case Rep 2011; 2011.
6. Del Chiaro M, Mucelli RP, Blomberg J, Segersvard R, Verbeke C. Is intraductal tubulopapillary neoplasia a new entity in the spectrum of familial pancreatic cancer syndrome? Fam Cancer 2014; 13(2): 227–229.
7. Motosugi U, Yamaguchi H, Furukawa T, Ichikawa T, Hatori T, Fujita I, Yamamoto M, Motoi F, Kanno A et al. Imaging studies of intraductal tubulopapillary neoplasms of the pancreas: 2-tone duct sign and cork-of-wine-bottle sign as indicators of intraductal tumor growth. J Comput Assist Tomogr 2012; 36(6): 710–717.
8. Cooper CL, O’Toole SA, Kench JG. Classification, morphology and molecular pathology of premalignant lesions of the pancreas. Pathology 2013; 45(3): 286–304.
9. Kasugai H, Tajiri T, Takehara Y, Mukai S, Tanaka JI, Kudo SE. Intraductal tubulopapillary neoplasms of the pancreas: case report and review of the literature. J Nippon Medl Sch 2013; 80(3): 224–229.
10. Kolby D, Thilen J, Andersson R, Sasor A, Ansari D. Multifocal intraductal tubulopapillary neoplasm of the pancreas with total pancreatectomy: report of a case and review of literature. Int J Clin Exp Pathol 2015; 8(8): 9672–9680.
11. Amato E, Molin MD, Mafficini A, Yu J, Malleo G, Rusev B, et al. Targeted next-generation sequencing of cancer genes dissects the molecular profiles of intraductal papillary neoplasms of the pancreas. J Pathol 2014; 233(3): 217–227.
12. Bledsoe JR, Shinagare SA, Deshpande V. Difficult diagnostic problems in pancreatobiliary neoplasia. Arch Pathol Lab Med 2015; 139(7): 848–857.
13. Kloppel G, Basturk O, Schlitter AM, Konukiewitz B, Esposito I. Intraductal neoplasms of the pancreas. Semin Diagn Pathol 2014; 31(6): 452–466.
14. Reid MD, Saka B, Balci S, Goldblum AS, Adsay NV. Molecular genetics of pancreatic neoplasms and their morphologic correlates: an update on recent advances and potential diagnostic applications. Am J Clin Pathol 2014; 141(2): 168–180.
15. Schlitter AM, Jang KT, Kloppel G, Saka B, Hong SM, Choi H, Offerhaus GJ, Hruban RH, Zen Y et al. Intraductal tubulopapillary neoplasms of the bile ducts: clinicopathologic, immunohistochemical, and molecular analysis of 20 cases. Mod Pathol. 2015; 28(9): 1249–1264.
16. Urata T, Naito Y, Nagamine M, Izumi Y, Tonaki G, Iwasaki H, Sasaki A, Yamasaki A, Minami N et al. Intraductal tubulopapillary neoplasm of the pancreas with somatic BRAF mutation. Clin J Gastroenterol 2012; 5(6): 413–420.
17. Yamaguchi H, Kuboki Y, Hatori T, Yamamoto M, Shimizu K, Shiratori K, Shibata N, Shimizu M, Furukawa T. The discrete nature and distinguishing molecular features of pancreatic intraductal tubulopapillary neoplasms and intraductal papillary mucinous neoplasms of the gastric type, pyloric gland variant. J Pathol 2013; 231(3): 335–341.
18. Yamaguchi H, Kuboki Y, Hatori T, Yamamoto M, Shiratori K, Kawamura S, Kobayashi M, Shimizu M, Ban S et al. Somatic mutations in PIK3CA and activation of AKT in intraductal tubulopapillary neoplasms of the pancreas. Am J Surg Pathol 2011; 35(12): 1812–1817.
19. Bhanot U, Basturk O, Berger M, Shah R, Scott S, Adsay V, Offerhaus GJ, Hruban RH, Zen Y et al. Molecular characteristics of the pancreatic intraductal tubulopapillary neoplasm. Mod Pathol 2015; 28(2S): 440A.
20. Springer S, Wang Y, Dal Molin M, Masica DL, Jiao Y, Kinde I, Blackford A4, Raman SP5, Wolfgang CL et al. A combination of molecular markers and clinical features improve the classification of pancreatic cysts. Gastroenterology 2015; 149(6): 1501–1510.
21. Hosoda W, Sasaki E, Murakami Y, Yamao K, Shimizu Y, Yatabe Y. BCL10 as a useful marker for pancreatic acinar cell carcinoma, especially using endoscopic ultrasound cytology specimens. Pathol Int 2013; 63(3): 176–182.
The authors
Shula Schechter MD; Jiaqi Shi* MD, PhD
Department of Pathology, University of Michigan,
Ann Arbor, MI 48109 USA
*Corresponding author
E-mail: jiaqis@med.umich.edu