Lipid testing and cardiovascular risk assessment: cut-off points
Dyslipidemia is one of the major risk factors for the development of cardiovascular disease (CVD). However, which lipoproteins to measure and what cut-off points to use in order to accurately assess this risk remains debatable.
by Mohamed S. Elgendy and Dr Mohamed B. Elshazly
Cardiovascular disease (CVD) mortality in the US in 2011 was estimated at 786 641 deaths representing approximately 33% of total annual deaths [1]. It remains the leading cause of mortality and morbidity in the developed world. Over many years of study, dyslipidemia has been identified as one of the major risk factors for developing CVD that can be modified through behavioral modifications as well as medications.
Lipoproteins
Lipoproteins are small particles formed of lipids and proteins, which play an important role in the transport and metabolism of cholesterol. Based on their relative density, they are divided into five major categories: high-density lipoprotein (HDL), low-density lipoprotein (LDL), intermediate density lipoprotein (IDL), very low-density lipoprotein (VLDL), and chylomicrons. LDL carries 60–70% of total serum cholesterol, HDL carries 20–30%, and VLDL carries 10–15% [2]. The remaining lipoproteins, namely triglyceride-rich lipoproteins such as VLDL, remnants and IDL, in addition to lipoprotein(a), carry a relatively small fraction of total cholesterol. Numerous studies have shown that LDL is the most atherogenic lipoprotein particle and lowering its levels has been the cornerstone of dyslipidemia management and CVD risk reduction in recent years. However, there is emerging evidence indicating that other lipoproteins also play a significant role in the process atherogenesis [23].
Relationship between lipoproteins and CVD risk
Several studies have reported a continuous relationship between LDL reduction and CVD risk reduction [3]. No threshold was identified below which a lower LDL concentration is not associated with lower risk [4]. For example, in the recent IMPROVE-IT trial, the incidence of CVD morbidity and mortality was lower in the ezetimibe/simvastatin group (with a median LDL-C follow-up of 53.7 mg/dL) compared to the simvastatin-alone group (with a median LDL-C follow-up of 69.5 mg/dL) [5]. In another study, individuals with hypobetalipoproteinemia, who have LDL-C levels less than 70 mg/dL, show prolonged longevity and very minimal rates of myocardial infarctions [6]. All of this supports the notion of ‘lower is better’.
LDL-C levels in the range of 25–60 mg/dL are considered physiologically adequate [7]. Even levels below 25 mg/dL have failed to show any adverse effects in a couple of recent trials [8, 9]. Although adverse effects of very low LDL, like hemorrhagic stroke and neurocognitive deficits, have been reported in some studies, they were neither significant nor consistent [10, 11]. Therefore, the benefits of achieving very low levels of LDL outweigh the risks. On the one hand, the lack of randomized clinical trials comparing the outcome of different LDL goals has made it difficult to reach a consensus among different guidelines on the optimal goals for high-risk patients or those with coronary disease equivalents with the commonly used target still being <70 mg/dL [12–14]. On the other hand, in the most recent American College of Cardiology (ACC)/American Heart Association (AHA) guidelines, targets were abandoned because of the notion that the benefit of statin is independent of LDL level [15]. Despite these differences, we believe that the conglomerate of evidence suggests that your LDL can never be too low although data examining patients with extremely low levels <25 mg/dL is still limited. The potential re-establishment of new even lower LDL targets in upcoming guidelines will require careful examination of data from proprotein convertase subtilisin kexin-9 (PCSK-9) trials to identify specific LDL levels below which risk outweighs benefit.
Other factors contribute to total atherogenic risk
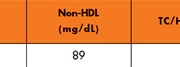
Despite the established recognition of LDL as the most atherogenic lipoprotein, it is not representative of total atherogenic risk. Elevated triglycerides were found to be associated with increased risk for CVD and this suggests that triglyceride-rich lipoproteins (TGRLs), especially the remnants, are atherogenic. These lipoproteins include VLDL, IDL, and chylomicrons (only in the non-fasting state). As LDL standard measurement by the Friedewald formula [Total cholesterol – HDL – triglycerides/5] [1] only includes LDL-C and lipoprotein(a), non-HDL has been proposed as a more inclusive parameter of atherogenic risk because it also incorporates VLDL-C, IDL-C and remnants in addition to LDL-C. In fact, several studies have demonstrated that non-HDL-C is more strongly associated with CVD than LDL-C and is a more powerful risk predictor [16–21]. Moreover, non-HDL measurement comes at no extra cost, as it is calculated from the standard lipid profile by subtracting HDL from total cholesterol, and does not require prior fasting. Nevertheless, due to the smaller number of studies examining non-HDL as a target of therapy, compared to that examining LDL, most of the current guidelines recommend non-HDL as a secondary target of therapy [2, 12, 14, 22]. Only the National Lipid Association recommends non-HDL as a primary target of therapy as well as LDL [22]. We believe this current situation represents a transitional phase toward using non-HDL as a primary target of therapy, just like the past transition from total cholesterol to LDL-C. This is most important when discordance exists between LDL and non-HDL levels within individuals, a relatively common finding particularly in patients with low LDL and high triglyceride levels [23]. The currently recommended non-HDL treatment goal is 30 mg/dL higher than that of LDL-C based on the rationale that ‘normal’ VLDL exists when triglycerides level is <150 mg/dL, which is <30 mg/dL [2]. However, in a recent study of 1.3 million US adults, non-HDL level of 93 mg/dL was percentile equivalent to LDL of 70 mg/dL [23] suggesting that a lower non-HDL goal should be targeted.
Particle-based measures such as apolipoprotein-B (Apo-B) and LDL particle concentration (LDL-P) also have the potential to replace cholesterol-based measures such as LDL or non-HDL as predictors of risk and targets of therapy. Apo-B constitutes the protein component of almost all the known atherogenic lipoproteins: VLDL, IDL, and LDL,;therefore, Apo-B measurement has been suggested to better estimate particle concentration, a more accurate reflection of subendothelial atherogenesis. Apo-B has been shown to be a better risk marker than LDL in multiple studies [17, 21, 24–29]. Many guidelines currently recommend Apo-B as an optional risk marker and target of therapy [12, 14, 22, 30]. Similarly, almost all the studies comparing LDL-P to LDL-C have shown superiority of particle concentration in terms of CVD risk assessment [31–34]. In the LUNAR trial and Framingham Offspring Study, there was a strong correlation between Apo-B and LDL-P with non-HDL, respectively, suggesting that non-HDL, available from the standard lipid profile, can be used satisfactorily for risk assessment [31, 35] keeping in mind that Apo-B may be superior in instances when discordance exists [36].
Whereas individual lipid parameters are important in risk prediction, summary estimates that assess the ratio of pro-atherogenic to anti-atherogenic lipoproteins also add important prognostic information regarding CVD risk. Out of the ratios that have been considered, total cholesterol to HDL cholesterol ratio (TC/HDL) and Apo-B/A1 are the most propitious. Despite TC/HDLs strong association with CVD risk [37–43], some have argued against any additional benefit this ratio might have, given that its two variables are included in estimating LDL by the Friedewald formula, in calculating non-HDL-C and in CVD risk estimation scores in addition to the contentiousness of HDL raising therapeutic strategies. However, in a recent 1.3 million population study, it has been documented that there is significant TC/HDL patient-level discordance in relation to LDL and non-HDL [44, 45]. This implies that TC/HDL may carry additional information reflecting atherogenic particle size and concentration [44, 45]. Notably, a TC/HDL ratio of 2.6 was percentile equivalent to an LDL level of 70 mg/dL (Table 1). Outcome data examining the clinical impact of TC/HDL discordance is still in progress and thus current guidelines do not currently recommend using TC/HDL.
Summary
There is no doubt that the field of dyslipidemia management has been one of the most dynamic fields in cardiology over the last 3 decades. With the recent advent of PCSK-9 inhibitors, we need to re-evaluate our understanding of lipoprotein reduction and ask ourselves important questions: Should guidelines re-establish treatment targets? What is the best lipoprotein parameter for predicting risk? Is it one parameter that is superior or is it the input of multiple parameters? What do we do when discordance between lipid parameters within individuals exists? Although a lot of data necessary to answer these questions is still a work in progress, recent data may be able to provide some insightful answers. First, LDL-C is not the optimal marker for total atherogenic risk. Second, instead of evaluating the performance of individual lipid parameters at a population level, we should evaluate their performance at an individual level where identifying discordance within individuals is key to understanding which marker may be superior. Third, particle-based measures such as Apo-B and LDL-P may be superior to cholesterol-based measures; however, summary estimates such as TC/HDL or Apo-B/A1 ratios also add significant information to individual parameters. Fourth, identifying new lipoprotein treatment goals is dependent on identifying certain lipoprotein levels below which risk may outweigh benefit. Therefore, it seems likely that a future where very low percentile-equivalent cut-off points of several lipoprotein parameters and ratios may be set as simultaneous goals for treatment.
References
1. Roger VL, Go AS, et al. Heart disease and stroke statistics–2012 update. Circulation 2012; 125(1): e2–220.
2. NCEP expert panel Third report of the National Cholesterol Education Program (NCEP) expert panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106(25): 3143–3143.
3. Boekholdt SM, Hovingh GK, et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol. 2014; 64(5): 485–94.
4. Law MR, Wald NJ, et al. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ 1994; 308(6925): 367–72.
5. Giugliano RP, Blazing MA. IMProved Reduction of Outcomes: Vytorin Efficacy International Trial. American College of Cardiology 2015;http://www.acc.org/latest-in-cardiology/clinical-trials/2014/11/18/16/25/improve-it
6. Glueck CJ, Gartside P, et al. Longevity syndromes: familial hypobeta and familial hyperalpha lipoproteinemia. J Lab Clin Med. 1976; 88(6): 941–957.
7. Brown MS, Goldstein JL. A receptor-mediated pathway for cholesterol homeostasis. Science 1986; 232(4746): 34–47.
8. Robinson JG, Farnier M, et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015; 372(16): 1489–1499.
9. Horton JD, Cohen JC, et al. PCSK9: a convertase that coordinates LDL catabolism. J Lipid Res. 2009; 50(Supplement): S172–177.
10. Law MR, Thompson SG, et al. Assessing possible hazards of reducing serum cholesterol. BMJ 1994; 308(6925): 373–379.
11. Hsia J, MacFadyen JG, et al. Cardiovascular event reduction and adverse events among subjects attaining low-density lipoprotein cholesterol <50 mg/dl with rosuvastatin: The JUPITER Trial (Justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin). J Am Coll Cardiol. 2011; 57(16): 1666–16675.
12. Genest J, McPherson R, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult – 2009 recommendations. Can J Cardiol. 2009; 25(10): 567–579.
13. Grundy SM, Cleeman JI, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004; 110(2): 227–239.
14. European Association for Cardiovascular Prevention & Rehabilitation, Reiner Ž, Catapano AL, et al. ESC/EAS Guidelines for the management of dyslipidaemias. Eur Heart J. 2011; 32(14): 1769–1818.
15. Stone NJ, Robinson JG, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129(25 Suppl 2): S1–45.
16. Bittner V, Hardison R, et al. Non-high-density lipoprotein cholesterol levels predict five-year outcome in the Bypass Angioplasty Revascularization Investigation (BARI). Circulation 2002; 106(20): 2537–2542.
17. Boekholdt S, Arsenault BJ, et al. Association of LDL cholesterol, non–HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: a meta-analysis. JAMA 2012; 307(12): 1302–1309.
18. Li C, Ford ES, et al. Serum non-high-density lipoprotein cholesterol concentration and risk of death from cardiovascular diseases among U.S. adults with diagnosed diabetes: the Third National Health and Nutrition Examination Survey linked mortality study. Cardiovasc Diabetol. 2011; 10: 46.
19. Liu J, Sempos CT, et al. Non–high-density lipoprotein and very-low-density lipoprotein cholesterol and their risk predictive values in coronary heart disease. Am J Cardiol. 2006; 98(10): 1363–1368.
20. Robinson JG, Wang S, et al. Meta-analysis of the relationship between non–high-density lipoprotein cholesterol reduction and coronary heart disease risk. J Am Coll Cardiol. 2009; 53(4): 316–322.
21. Sniderman AD, Williams K, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes 2011; 4(3): 337–345.
22. Jacobson TA, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;http://linkinghub.elsevier.com/retrieve/pii/S1933287415003803
23. Elshazly MB, Martin SS, et al. Non–high-density lipoprotein cholesterol, guideline targets, and population percentiles for secondary prevention in 1.3 million adults: The VLDL-2 Study (very large database of lipids). J Am Coll Cardiol. 2013; 62(21): 1960–1965.
24. Jiang R, Schulze MB, et al. Non-HDL cholesterol and apolipoprotein B predict cardiovascular disease events among men with type 2 diabetes. Diabetes Care 2004; 27(8): 1991–1997.
25. Shai I, Rimm EB, et al. Multivariate assessment of lipid parameters as predictors of coronary heart disease among postmenopausal women: potential implications for clinical guidelines. Circulation 2004; 110(18): 2824–2830.
26. Sniderman A, Williams K, et al. Non-HDL C equals apolipoprotein B: except when it does not! Curr Opin Lipidol. 2010; 21(6): 518–524.
27. Talmud PJ, Hawe E, et al. Nonfasting apolipoprotein B and triglyceride levels as a useful predictor of coronary heart disease risk in middle-aged UK men. Arterioscler Thromb Vasc Biol. 2002; 22(11): 1918–1923.
28. Walldius G, Jungner I. Apolipoprotein B and apolipoprotein A-I: risk indicators of coronary heart disease and targets for lipid-modifying therapy. J Intern Med. 2004; 255(2): 188–205.
29. Walldius G, Jungner I, et al. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. The Lancet 2001; 358(9298): 2026–2033.
30. Grundy SM, Arai H, et al. An International Atherosclerosis Society position paper: global recommendations for the management of dyslipidemia – full report. J Clin Lipidol. 2014; 8(1): 29–60.
31. Cromwell WC, Otvos JD, et al. LDL particle number and risk of future cardiovascular disease in the Framingham Offspring Study – implications for LDL management. J Clin Lipidol. 2007; 1(6): 583–592.
32. El Harchaoui K, van der Steeg WA, et al. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007; 49(5): 547–553.
33. Mora S, Otvos JD, et al. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation 2009; 119(7): 931–939.
34. Otvos JD, Mora S, et al. Clinical implications of discordance between LDL cholesterol and LDL particle number. J Clin Lipidol. 2011; 5(2): 105–113.
35. Ballantyne CM, Pitt B, et al. Alteration of relation of atherogenic lipoprotein cholesterol to apolipoprotein B by intensive statin therapy in patients with acute coronary syndrome (from the Limiting UNdertreatment of lipids in ACS With Rosuvastatin [LUNAR] trial). Am J Cardiol. 2013; 111(4): 506–509.
36. Mora S. Advanced lipoprotein testing and subfractionation are not (yet) ready for routine clinical use. Circulation 2009; 119(17): 2396–404.
37. Prospective Studies Collaboration, Lewington S, Whitlock G, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 2007; 370(9602): 1829–1839.
38. Ingelsson E, Schaefer EJ, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA 2007; 298(7): 776–785.
39. Manickam P, Rathod A, et al. Comparative prognostic utility of conventional and novel lipid parameters for cardiovascular disease risk prediction: do novel lipid parameters offer an advantage? J Clin Lipidol. 2011; 5(2): 82–90.
40. Kastelein JJP, Steeg WA van der, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation 2008; 117(23): 3002–3009.
41. McQueen MJ, Hawken S, et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet 2008; 372(9634): 224–233.
42. Mora S, Otvos JD, et al. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation 2009; 119(7): 931–939.
43. Ridker PM, Rifai N, et al. Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA 2005; 294(3): 326–333.
44. Elshazly MB, Quispe R, et al. Patient-level discordance in population percentiles of the total cholesterol to high-density lipoprotein cholesterol ratio in comparison with low-density lipoprotein cholesterol and non–high-density lipoprotein cholesterol: The Very Large Database of Lipids Study (VLDL-2B). Circulation.2015; 132(8): 667–676.
45. Friedewald WT, Levy RI, et al. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18(6): 499–502.
The authors
Mohamed S. Elgendy1 and Mohamed B. Elshazly*2 MD
1Kasr Al Ainy School of Medicine, Cairo University, Cairo, Egypt
2Cleveland Clinic, Heart and Vascular Institute, Cleveland, OH 44195, USA
*Corresponding author
E-mail: elshazm@ccf.org