New screening strategies in prenatal care by the introduction of non-invasive prenatal testing for fetal aneuploidies
The identification of cell-free fetal DNA (cffDNA) in maternal plasma has led to the development of non-invasive prenatal testing (NIPT) for fetal aneuploidies risk assessment. The high accuracy of NIPT has profoundly influenced the field of prenatal care.
by F. Gerundino, Dr C. Giachini, C. Giuliani, E. Contini and Dr E. Pelo
Background
Several well-established screening approaches to estimate the personal risk for common autosomal aneuploidies such as trisomy 21 (T21, Down syndrome), trisomy 18 (T18, Edwards syndrome) and trisomy 13 (T13, Patau syndrome) are part of the standard prenatal care in many countries. These approaches are based on the combination of different parameters such as maternal age, markers in maternal serum and ultrasound findings in the first or second trimester of pregnancy. Overall, conventional screening tests show a detection rate (DR) of 80–95% with a high false positive rate (FPR) (3–5%). Pregnancies identified to be at high risk (using locally established cut-off values) are offered invasive prenatal diagnosis (IPD) to provide a definitive result. IPD, carried out using either chorionic villus sampling (CVS) or amniocentesis to obtain fetal cells, is associated with an estimated miscarriage risk of 0.5–1% [1]. Given the FPR of conventional screening protocols a not negligible number of pregnancies undergo unnecessary IPD. The identification of cell-free fetal DNA (cffDNA) in plasma of pregnant women [2] has opened new possibilities to improve non-invasive prenatal screening of common fetal aneuploidies. In the last decade, several groups developed massively parallel sequencing (MPS) – using targeted or whole genome approaches – of cell-free DNA (cfDNA) from maternal plasma to detect fetal aneuploidies [3, 4]. These approaches, referred to as non-invasive prenatal testing (NIPT) or non-invasive prenatal screening (NIPS), have been shown to outperform traditional screening protocols. According to a recent meta-analysis, the DR of NIPT was 99.2% for T21, 96.3%, 91.0% and 90.3% for T18, T13 and monosomy X, respectively; the FPR was below 1% for all of these aneuploidies [5]. Since 2011, NIPT became commercially available in the USA and China and was rapidly introduced into standard prenatal care in many countries.
Cell-free-DNA-based screening: validation of a method for fetal aneuploidies risk
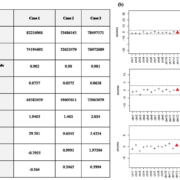
The conventional first-trimester screening (FTS) is currently offered to all pregnant women by the public health system in Tuscany. Recently, we validated a NIPT method based on whole genome MPS approach [6], in order to introduce a more robust screening test within the public health system. In whole genome approach, maternal and fetal DNA fragments (called reads) are sequenced simultaneously in a single run. Sequence reads were aligned to specific chromosome locations within the human genome and the number of reads mapped to the chromosome of interest are counted. A relative increase or decrease in the number of reads respect to a predefined threshold value (Z-score) reveals a potential risk of aneuploidy for a specific chromosome. In particular, a trisomy was called when Z-score >3 (Fig. 1). MPS was performed on a total of 381 cfDNA samples isolated from maternal plasma by two steps: a first set of 186 euploid samples was analysed to generate a preliminary reference dataset (group A) and a second set of 195 samples (group B) – enriched by 69 aneuploid cases – was analysed in blind versus the reference dataset to verify the reliability of our sequencing protocol as well as the analysis method. One hundred and fifty samples from group A (80.6%) and 177 samples from group B (90.8%) gave resulted suitable (>10×106 mapped reads) for downstream data analysis. The two groups (A and B) were then merged to generate a definitive dataset (n=327), which was then used to re-analyse the whole study population. Since the fetal fraction (FF) (i.e. the proportion of fetal DNA to the total cfDNA in maternal plasma) is a parameter that strictly influences NIPT performance [7], a droplet digital PCR (ddPCR) protocol has been validated for its assessment [8]. FF quantification by ddPCR was performed in 178/381 (46.7%) samples after methylation-sensitive DNA digestion. Absolute quantification of both fetal (on digested RASSF1A) and total DNA (on TERT and undigested beta-actin/RASSF1A) was calculated as the ratio between the average copies/µL of fetal DNA and total DNA. An SRY assay was used for fetal gender assessment [6].
Results of the validation study
Considering the performance of the definitive reference dataset, all positive samples for T21 (n=43), T18 (n=6) and T13 (n=7) were correctly identified (sensitivity 99.9%). Five false positive (FP) results were observed: three for T21 (specificity 98.9%) and two for T13 (specificity 99.4%).
Z-score values of true positive (TP) cases for T21 and T13 were always higher than 4.6 and 6.6, respectively. Conversely, all Z-score values of FP cases for T21 and T13 lay within 3.0 and 4.0 (the so-called Z-score ‘grey zone’). Sex chromosome status was correctly assigned in 317/324 (97.8%) cases: 166 males, 149 females and 2 cases with monosomy X. In 3/327 (0.9%) samples fetal gender could not be assigned because of an inconclusive result in data analysis. Seven discordant cases between MPS and follow-up data were observed. The only case of false negative (FN) male has been explained by a low FF (0.3%), underling the importance of FF determination. Only two out of four cases with monosomy X were correctly identified by NIPT, while the remaining two cases were erroneously classified as male.
Discussion
NIPT is an accurate screening test without associated risk for the mother and/or the fetus and it can be performed early in pregnancies, starting from 9–10 weeks of gestation. It is suitable both in low- and high-risk pregnancies, even if the positive predictive value (PPV) of the test (the chance that the positive result is a true positive) is lower in low risk cohorts. Two large studies show that in the general population NIPT outperforms conventional screening tests for T21 with a PPV ranging from 45.5 to 80.9% versus a PPV of 3.4–4.2% [9, 10]. Pre- and post-test counselling to inform patients about benefits, risks, test failure and testing alternatives should be provided before offering cfDNA screening. Owing to a series of intrinsic limitations, NIPT cannot be considered a diagnostic tool, despite its high performance. In the management of pregnancies with a high-risk NIPT, the possibility of FP results should always be taken into account and IPD should be recommended after a NIPT-positive result. cffDNA derives from the apoptosis of the placental cytotrophoblast cells, therefore in rare cases it may not represent the genetic constitution of the fetus. FP results may arise from confined placental mosaicism (CMP) in which some or all trophoblastic cells are trisomic, whereas the fetus is normal (1–2% of first-trimester placentas) [11]. FN results are a very rare occurrence and can be explained by fetoplacental discrepancies, in which the fetus shows an abnormal karyotype but the chromosome aberration is absent in the cytotrophoblast and, therefore, in the cffDNA. Additional sources of FP results can be unanticipated finding such as maternal chromosome abnormalities (maternal mosaicisms, microdeletions and other copy-number variations) or maternal malignancy, or the presence of a vanishing twin with an early loss of a trisomic fetus.
Failure to provide a result occurs in 1.6–6.4% of NIPT. Both laboratory technical issues or low FF can cause the failure [12]. Low FF in frequently found in overweight pregnant women, in which the low FF could be due to a dilution effect of an increased blood volume or to the high turn-over of adipocytes [13]. In these cases it is not advisable to repeat the test on a new sample because the probability of a second test failure is quite high. An accurate clinical management of cases with low FF and normal maternal weight is instead recommended, because FF is lower in pregnancies with aneuploid fetuses (T18, T13, monosomy X and triploidy) compared to euploid pregnancies [14].
NIPT has rapidly spread in many countries through commercial provider, leading to a re-examination of current screening methods, and several models of implementation of NIPT have been proposed with pros and cons. Current guidelines recommend that “in countries where prenatal screening is offered as a public health service, governments and public health authorities should assume an active role to ensure the responsible introduction of NIPT” [15].
Our study represents the first experience of NIPT within the Italian public health system. Following our validation study, NIPT testing for T21, T13 and T18 has been introduced as a clinical service for all pregnant women after 10+4 week of gestation upon payment. Our regional health system has planned a pilot study of two years to evaluate the benefit-to-cost ratio of NIPT introduction into routine prenatal care to support the current screening strategy based on nuchal translucency measurement and maternal serum biomarker quantification. NIPT will be offered in an adequate context of pre- and post-test counselling as an alternative option to IPD in pregnant women with high risk after FTS and applying the national cut-off of 1:250. We expect that this strategy would lead to a significant reduction in unnecessary IPD due to FP results of FTS with a reduction in fetal losses associated to diagnostic procedures among high-risk women, allowing us to offer the best screening strategy currently available.
References
1. Tabor A, Alfirevic Z. Update on procedure-related risks for prenatal diagnosis techniques. Fetal Diagn Ther 2010; 27(1): 1–7.
2. Lo YM, Corbetta N, Chamberlain PF, Rai V, Sargent IL, Redman CW, Wainscoat JS. Presence of fetal DNA in maternal plasma and serum. Lancet 1997; 350(9076): 485–487.
3. Chiu RW, Chan KC, Gao Y, Lau VY, Zheng W, Leung TY, Foo CH, Xie B, Tsui NB, et al. Noninvasive prenatal diagnosis of fetal chromosomal aneuploidy by massively parallel genomic sequencing of DNA in maternal plasma. Proc Natl Acad Sci U S A 2008; 105(51): 20458–20463.
4. Fan HC, Blumenfeld YJ, Chitkara U, Hudgins L, Quake SR. Noninvasive diagnosis of fetal aneuploidy by shotgun sequencing DNA from maternal blood. Proc Natl Acad Sci U S A 2008; 105(42): 16266–16271.
5. Gil MM, Quezada MS, Revello R, Akolekar R, Nicolaides KH. Analysis of cell-free DNA in maternal blood in screening for fetal aneuploidies: updated meta-analysis. Ultrasound Obstet Gynecol 2015; 45(3): 249–266.
6. Gerundino F, Giachini C, Contini, E Benelli M, Marseglia G, Giuliani C, Marin F, Nannetti G, Lisi E, et al. Validation of a method for noninvasive prenatal testing for fetal aneuploidies risk and considerations for its introduction in the Public Health System. J Matern Fetal Neonatal Med 2017; 30(6): 710–716.
7. Palomaki GE, Kloza EM, Lambert-Messerlian GM, Haddow JE, Neveux LM, Ehrich M, van den Boom D, Bombard AT, Deciu C, et al. DNA sequencing of maternal plasma to detect Down syndrome: an international clinical validation study. Genet Med 2011; 13(11): 913–920.
8. Chan KC, Ding C, Gerovassili A, Yeung SW, Chiu RW, Leung TN, Lau TK, Chim SS, Chung GT, et al. Hypermethylated RASSF1A in maternal plasma: A universal fetal DNA marker that improves the reliability of noninvasive prenatal diagnosis. Clin Chem 2006; 52(12): 2211–2218.
9. Bianchi DW, Parker RL, Wentworth J, Madankumar R, Saffer C, Das AF, Craig JA, Chudova DI, Devers PL, et al. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med 2014; 370(9): 799–808.
10. Norton ME, Jacobsson B, Swamy GK, Laurent LC, Ranzini AC, Brar H, Tomlinson MW, Pereira L, Spitz JL, et al. Cell-free DNA analysis for noninvasive examination of trisomy. N Engl J Med 2015; 372(17): 1589–1597.
11. Kalousek DK, Vekemans M. Confined placental mosaicism. J Med Genet 1996; 33(7): 529–533.
12. Yaron Y. The implications of non-invasive prenatal testing failures: a review of an under-discussed phenomenon. Prenat Diagn 2016; 36(5): 391–396.
13. Haghiac M, Vora NL, Basu S, Johnson KL, Presley L, Bianchi DW, Hauguel-de Mouzon S. Increased death of adipose cells, a path to release cell-free DNA into systemic circulation of obese women. Obesity 2012; 20(11): 2213–2219.
14. Rava RP, Srinivasan A, Sehnert AJ, Bianchi DW. Circulating fetal cell-free DNA fractions differ in autosomal aneuploidies and monosomy X. Clin Chem 2014; 60(1): 243–250.
15. Dondorp W, de Wert G, Bombard Y, Bianchi DW, Bergmann C, Borry P, Chitty LS, Fellmann F, Forzano F, et al. Non-invasive prenatal testing for aneuploidy and beyond: challenges of responsible innovation in prenatal screening. Summary and recommendations. Eur J Hum Genet 2015; doi: 10.1038/ejhg.2015.56.
The authors
Francesca Gerundino BS, Claudia Giachini PhD, Costanza Giuliani BS, Elisa Contini BS, Elisabetta Pelo* MD
Diagnostic Genetic Unit, Careggi University Hospital, Florence, Italy
*Corresponding author
E-mail: peloe@aou-careggi.toscana.it