Overview of biomarkers for predicting Alzheimer’s disease
The two aims of this article are to review some current methods of early diagnosis of Alzheimer’s disease (AD) and to discuss a new integration method proposed in Kong et al. [1]. We focus on how to combine the whole genome single nucleotide polymorphism (SNP) data and high-dimensional whole-brain imaging data to offer predictive values to identify subjects at risk for progressing to AD.
by Dr Dehan Kong, Prof. Kelly S. Giovanello, Eunjee Lee, Prof. P. Murali Doraiswamy and Prof. Hongtu Zhu
Introduction
Mild cognitive impairment (MCI), which commonly arises as a result of underlying neurodegenerative pathology, is a clinical syndrome characterized by insidious onset and gradual progression. Recently, much research has focused on delineating a set of biomarkers that provide evidence of such neurodegenerative pathology in living individuals and increasing attention has been devoted to combine the information from imaging, genetic, clinical, behavioural and fluid data to predict the conversion from MCI to AD. In this article, we first review some of the literature on MCI-to-AD conversion and their limitations. Subsequently, we review the results in Kong et al. [1]. According to the best of our knowledge, it is the first paper that addresses the question of how to combine the whole genome single nucleotide polymorphism (SNP) data and high-dimensional whole-brain imaging data to offer predictive values to identify subjects at risk for progressing to AD.
Methods for predicting progression from MCI to AD
There are several studies assessing the relative importance of different modalities in predicting the diagnostic change from MCI to AD by using a small subset of biosignatures [2–6]. For example, Cui et al. simultaneously examined multiple features from different modalities of data [2]. In particular, they combined structural magnetic resonance imaging (MRI) morphometry, cerebrospinal fluid biomarkers and neuropsychological measures to access an optimal set of predictors of conversion from MCI to AD. Their findings suggested that structural changes within the medial temporal lobe (MTL), particularly the hippocampus, and the performance on cognitive tests that rely on MTL integrity provided strong prediction for MCI-to-AD conversion.
Recent studies focused on the analysis of longitudinal data to assess the dynamic changes of various biomarkers associated with the MCI-to-AD conversion. A prominent neural correlate of MCI–AD is volume loss within the MTL, especially within the hippocampus and entorhinal cortex [7, 8], with increasing atrophy in these structures from normal aging to MCI to AD [9, 10]. The importance of assessing MTL changes in tracking the progression of MCI to AD has been highlighted in various longitudinal studies of individuals with MCI-AD conversion. For instance, an increased likelihood of progressing to clinical dementia has been linked with documented diminished baseline hippocampal and entorhinal volumes in several studies [11, 12].
The aforementioned studies focused on the question of whether the MCI subjects progress to AD or not, i.e. treating the conversion as a binary response. However, an important question remains, namely, how can we predict the time to conversion in MCI individuals, as well as determine the early markers of conversion? In Tarbert et al., the authors used 148 MCI subjects to identify the most predictive neuropsychological measures [13]. In Li et al., the authors used 139 MCI subjects from the Alzheimer’s disease neuroimaging initiative phase 1 (ADNI-1) to evaluate the prediction power of brain volume, ventricular volume, hippocampus volume, apolipoprotein E (APOE) gene status, cerebrospinal fluid (CSF) biomarkers, and behavioural scores [14]. They found that baseline volumetric MRI and behavioural scores were selectively predictive, and their model can achieve a moderately accurate prediction with the value of an area under the curve of 0.757 at 36 months. In Da et al., the authors used 381 MCI subjects from ADNI-1 to evaluate how several biomarkers for predicting MCI-to-AD conversion including spatial patterns of brain atrophy, Alzheimer’s disease assessment scale-cognitive subscale (ADAS-Cog) score, APOE genotype, and cerebrospinal fluid (CSF) biomarkers [15]. They have found that a combination of spatial patterns of brain atrophy and ADAS-Cog score offers a good predictive power of conversion from MCI to AD.
To the best of our knowledge, none of the previous studies have leveraged both genome-wide association study (GWAS) SNP data as well as high-dimensional whole-brain imaging data to examine their combined value in identifying subjects at greatest risk for progressing to AD.
Predicting AD using combined imaging–whole genome SNP data
In Kong et al., the authors focused on the MCI patients and combined information from whole brain MR imaging and whole genome data to predict the time to onset of AD in a 48-month national study of subjects at risk [1]. This study considered 343 subjects with MCI enrolled in ADNI-1. The patients were followed over 48 months, with 150 participants progressing to AD. The data can be treated as time-to-event data before those MCI subjects without conversion are censored data. One of the most popular models for the time-to-event data is the Cox proportional hazards model. The authors used this model to account for the covariates that are associated with the time of the events, i.e. conversion from MCI to AD.
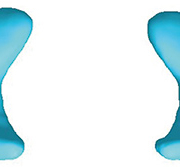
The candidate covariates include demographic covariates (age, gender, handedness, mean education length, retirement percentage, and three dummy variables for the marital status), the APOE4 genotype, the AD assessment scale-cognitive subscale (ADAS-Cog) score, the hippocampus surface data, the region of interest (ROI) volume data, the chromosome-wise information and the significant SNP information. For each subject, the radial distance was obtained from the baseline hippocampal surfaces data for each subject, which yielded two sets of 15 000 dimensional vectors denoting the surface data from both parts of the hippocampus. For better illustration, we have plotted the hippocampus surface in Figure 1.
In Kong et al., the authors treated each part of the hippocampi as a functional predictor, and applied functional principal component analysis, and selected seven functional principal component scores for each functional predictor, which explain approximately 70% of the variance [1]. These functional principal component scores were taken as the summary measures for the hippocampus surface and put into the Cox regression model as predictors. For the chromosome-wise information, they extracted the top two principal components of the SNP data along each chromosome as predictors. For the significant SNP information, the top 101 significant SNPs were picked up using a kernel machine method, and then their top five principal components (PCs) were calculated and been used as predictors.
Specifically, they considered three candidate models. The first model is to fit a Cox regression model with demographic, clinical and ADAS-Cog score as predictors as well as APOE. This model did not include any other imaging and genetic data. The second model is to fit a Cox regression model with demographic, imaging and chromosome-wise predictors, but without the ADAS-Cog score and significant SNPs information. As a comparison, they also considered the genetic information from genome-wide association analysis (GWAS). The third model is to fit a Cox regression model with demographic, imaging and significant SNP information, but without the ADAS-Cog score and chromosome-wise information.
They compared the predictive value of the first and second model, and receiver operating characteristic (ROC) analysis indicated that the first model had a lower predictive value at 48 months than the second model. For the first model, they only identified APOE4 and ADAS-Cog score as the significant predictors. For the second model, they found that combining full genetic SNP and high-dimensional imaging data had a much higher predictive value. In particular, SNPs on chromosomes 2, 10, 11, 15, 17 and 18, APOE4 genotype, surface morphology data of both hippocampi and volumes of hippocampus, amygdala and thalamus contributed significantly. The findings support those from previous MRI studies of volumetric hippocampal changes in prodromal AD and extend them by finding that the possible prognostic value of combining information from high-dimensional imaging and genetics may be superior to that provided by routine clinical cognitive testing data. The findings also confirm the association between APOE4 status and AD, and identify additional new markers on chromosomes 2, 10, 11, 15, 17 and 18 as significant predictors for conversion. For the third model, they found that the predictive value is lower than that of the second model. This finding indicates that using the chromosome-wise information instead of the traditional significant SNPs information would be favoured. They suggest it may be due to the pitfalls of prediction using significant SNPs [16].
There are some limitations to their analysis. First, there are no test data for this study, and their findings are based on the interval cross validation. Second, they did not include measures of pathology in the models, as cerebrospinal fluid and amyloid-PET were available only in a small subset of individuals in ADNI-1. It would be beneficial to combine the data from ADNI-GO and ADNI-2 for future research.
Summary
In this article, we first reviewed some current methods of diagnosis of AD, and discussed their limitations. Then we reviewed the method and findings in Kong et al. and discussed the novelty and advantages of their study and how their proposal can be used for early diagnosis of AD by combined imaging–whole genome SNP data [1].
Acknowledgements
This material was based upon work partially supported by the NSF grant DMS-1127914 to the Statistical and Applied Mathematical Science Institute. The research of Dr Zhu was supported by NSF grants SES-1357666 and DMS-1407655 and NIH grants MH086633, T32MH106440, and 1UL1TR001111. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH and NSF.
References
1. Kong D, Giovanello KS, Wang Y, Lin W, Lee E, Fan YD Doraiswamy PM, Zhu H, Alzheimer’s Neuroimaging Initiative. Predicting Alzheimer’s disease using combined imaging-whole genome SNP data. J Alzheimer’s Dis. 2015; 46(3): 695–702.
2. Cui Y, Liu B, Luo S, Zhen X, Fan M, Liu T, Zhu W, Park. M, Jiang T, Jin SE. Identification of conversion from Mild Cognitive Impairment to Alzheimer’s disease using multivariate predictors. PLoS One 2011; 6: e21896.
3. Davatzikos C, Bhatt P, Shaw LM, Batmanghelich KN, Trojanowski JQ. Prediction of MCI to AD conversion, via MRI, CSF biomarkers, and pattern classification. Neurobiol Aging 2011; 32: 2322.e19–2322.e27.
4. Dickerson BC, Wolk DA, Alzheimer’s Disease Neuroimaging Initiative. Biomarker-based prediction of progression in MCI: comparison of AD signature and hippocampal volume with spinal fluid amyloid-β and tau. Front Aging Neurosci. 2013; 5: 1–9.
5. Young J, Modat M, Cardoso MJ, Mendelson A, Cash D, Ourselin S. Accurate multimodal probabilistic prediction of conversion to Alzheimer’s disease in patients with mild cognitive impairment. Neuroimage Clin. 2013; 2: 735–745.
6. Zhang D, Shen D. Predicting future clinical changes of MCI patients using longitudinal and multimodal biomarkers. PLoS One 2012; 7(3): e33182.
7. Dickerson BC, Goncharova I, Sullivan MP, Forchetti C, Wilson RS, Bennett DA, Beckett LA, deToledo-Morrell L. MRI-derived entorhinal and hippocampal atrophy in incipient and very mild Alzheimer’s disease. Neurobiol Aging 2001; 22: 747–754.
8. Xu Y, Jack CR, O’Brien PC, Kokmen E, Smith GE, Ivnik RJ, Boeve BF, Tangalos RG, Petersen RC. Usefulness of MRI measures of entorhinal cortex versus hippocampus in AD. Neurology 2000; 54: 1760–1767.
9. Du AT, Schuff N, Amend D, Laakso MP, Hsu YY, Jagust WJ, et al. Magnetic resonance imaging of the entorhinal cortex and hippocampus in mild cognitive impairment and Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2001; 71: 441–447.
10. Pennanen C, Kivipelto M, Tuomainen S, Hartikainen P, Hanninen T, Laakso MP, et al. Hippocampus and entorhinal cortex in mild cognitive impairment and early AD. Neurobiol Aging. 2004; 25: 303–310.
11. Jack CR, Petersen RC, Xu YC, O’Brien PC, Smith GE, Ivnik RJ, Boeve BF, Waring SC, Tangalos EG, Kokmen E. Prediction of AD with MRI-based hippocampal volume in mild cognitive impairment. Neurology 1999; 52: 1397–1403.
12. Killiany RJ, Gomez-Isla T, Moss M, Kikinis R, Sandor T, Jolesz F, et al. Use of structural magnetic resonance imaging to predict who will get Alzheimer’s disease. Ann Neurol. 2000; 47:430–439.
13. Tabert MH, Manly JJ, Liu X, Pelton GH, Rosenblum S, Jacobs M, Zamora D, Goodkind M, Bell K, Stern Y, Devanand DP. Neuropsychological prediction of conversion to Alzheimer disease in patients with mild cognitive impairment. Arch Gen Psychiatry. 2006; 63(8): 916–24.
14. Li S, Okonkwo O, Albert M, Wang M-C. Variation in variables that predict progression from MCI to AD dementia over duration of follow-up. American J Alzheimer’s Dis. 2013; 1: 12–28.
15. Da X, Toledo JB, Zee J, Wolk DA, Xie SX, Ou Y, Shacklett A, Parmpi P, Shaw L, Trojanowski JQ, Davatzikos C, Alzheimer’s Neuroimaging Initiative. Integration and relative value of biomarkers for prediction of MCI to AD progression: Spatial patterns of brain atrophy, cognitive scores, APOE genotype and CSF biomarkers. Neuroimage Clin. 2014; 4: 164–173.
16. Wray NR, Yang J, Hayes BJ, Price AL, Goddard ME and Visscher PM. Pitfalls of predicting complex traits from SNPs. Nat Rev Genet 2013; 14(7): 507–15.
The authors
Dehan Kong1 PhD, Kelly S. Giovanello2,3 PhD, Eunjee Lee4 MS, P. Murali Doraiswamy5 MD, Hongtu Zhu*1,3,6 PhD
1 Department of Biostatistics, University of North Carolina (UNC), NC, USA
2 Department of Psychology, UNC, NC, USA
3 Biomedical Research Imaging Center, UNC, NC, USA
4 Department of Statistics, UNC, NC, USA
5 Departments of Psychiatry and Duke Institute for Brain Sciences, Duke University, Durham, NC, USA
6 Department of Radiology, UNC, NC, USA
*Corresponding author
E-mail: htzhu@email.unc.edu