Respiratory infections due to non-diphtheriae Corynebacterium species
Some species of non-diphtheriae Corynebacterium bacteria are opportunistic pathogens responsible for lower respiratory tract infections primarily in immunocompromised patients or in patients with chronic respiratory diseases. In the last years an increasing number of reports have demonstrated their role as emerging pathogens causing pneumonia or exacerbations of chronic pulmonary diseases. Thus, these species should not always be considered as mere colonizers.
by Dr M. Díez-Aguilar, Dr R. Cantón, Dr M. A. Meseguer
Non-diphtheriae Corynebacterium species are considered to be colonizers of the skin, nasopharyngeal tract and mucous membranes. However, in the last decade there have been an increasing number of reports that recognize these microorganisms as opportunistic pathogens that can cause disease in certain circumstances [1–3]. Since the population of immunocompromised patients is constantly growing, due to AIDS, age, use of invasive devices and immunosuppressive regimens, e.g. after transplantation, the clinical relevance of these opportunistic pathogens is rising.
A broad range of infectious diseases caused by non-diphtheriae Corynebacterium species have been reported including endocarditis, bacteriemia, pneumonia, tracheobronchitis, necrotizing tracheitis, exudative pharyngitis, rhinosinusitis, osteitis, conjunctivitis, and skin and urinary tract infections.
Lower respiratory tract infection, typically occurs in the context of underlying immunosuppressive conditions (such as diabetes, malignancy, corticoid therapy) and in patients with pre-existing pulmonary diseases such as chronic obstructive pulmonary disease (COPD), bronchiectasis and cystic fibrosis. In these patients non-diphtheriae Corynebacterium species can cause pneumonia and acute exacerbations of COPD. Previous hospitalization, wide-ranged antibiotic therapy and presence of multiple medical devices are risk factors for acquiring non-diphtheriae corynebacterial infection. Nosocomial outbreak of infection or colonization has been also observed [4]. Nevertheless, community acquired bronchitis in elderly patients with COPD have been reported.
Typically, Corynebacterium pseudodiphtheriticum, Corynebacterium striatum, and Corynebacterium propinquum are the species more frequently involved in lower respiratory tract infections [1–4]. The role of other Corynebacterium species in lower respiratory tract infections could have been underestimated, as only a few cases have been reported. The various non-diphtheriae Corynebacterium species that have been involved as responsible for respiratory tract infections are shown in Table 1. After appropriate antibiotic treatment a favourable outcome was achieved in most patients.
Pathogenesis
The respiratory tract damage caused by these microorganisms is probably the result of their opportunistic overgrowth and their possible virulence factors in patients with immune impairment and/or compromised pulmonary function.
Patients with chronic respiratory infections, such as obstructive pulmonary disease and bronchiectasis are predisposed to a persistent and non-innocent colonization of the lower respiratory tract by several non-pathogenic microorganisms. The high density of microorganisms covering the surface of the bronchial mucosa results in consistent pathogenic effects throughout the respiratory epithelium. Such effects include reduction of the supply of oxygen, water and organic nutrients to cells of the bronchial epithelium, as well as the liberation of potentially bioactive molecules which induce pro-inflammatory processes leading to accumulation of immune inflammatory cells. Defective pulmonary defences (impaired mucociliary clearance, airway inflammation and permanent dilatation within the bronchial wall), periodic infectious exacerbations caused by other respiratory infecting pathogens, and local immune disorders can cause a ‘vicious cycle’ of infection and inflammation of the airway. In these conditions the replacement of the pharyngeal resident microbiota with the opportunistic overgrowth and predominance of corynebacterial organisms in the respiratory tract can take place resulting in disease.
However, these microorganisms could express virulence factors that would contribute to the infection. Still, the virulence factors of non-diphtheriae Corynebacterium infection remain poorly understood, but recent in vitro studies on Corynebacterium pseudodiphtheriticum behaviour with epithelial cells have demonstrated the capacity for adherence, internalization, intracellular survival and persistence of the organism [5]. Therefore, in vivo C. pseudodiphtheriticum not only multiplies at and remains on the surface of the epithelial host cells, but also could reach the cytoplasm. This ability of C. pseudodiphtheriticum to survive within host cells highlights the potential capacity of other non-diphtheriae Corynebacterium to act as opportunistic pathogens.
Microbiological diagnosis
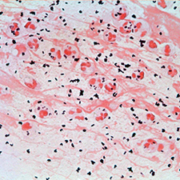
The key for the microbiological diagnosis of respiratory tract infection caused by non-diphtheriae Corynebacterium species is the microscopic observation of the predominant presence of Corynebacterium morphotype in a Gram stained purulent respiratory sample [Fig. 1], together with an abundant growth in the culture [6]. To determine the quality of the sputum it is important to follow the scoring system of Washington and Murray, which assesses a good quality of samples when there are more than 25 leukocytes and less than 10 squamous epithelial cells per field.
Identification of Coryneform bacteria
It is important to correctly identify Coryneform bacteria to the species level in order to reach the microbiological diagnosis, but also to detect unsuspected species, investigate potential pathogenicity and describe new species that could be clinically relevant.
Phenotypic characteristics such as colony size, pigmentation, catalase, and motility are useful for establishing the genus. For identification to the species level, biochemical testing performed using commercially available identification systems such as API Coryne, API CH50 plus, API 20 E and Rap IDCB Plus method, as well as automated systems such as Vitek2 (bioMèriux) and Biology systems could be employed. However, these methods are unreliable for some species (Corynebacterium accolens, C. striatum).
Nowadays an accurate and definitive identification is reached by the use of sequence-based identification techniques: 16s RNA and rpoB gene are the two approaches used for the characterization of non-diphtheriae Corynebacterium species. In fact, in recent years, many new species of the Corynebacterium genus have been described thanks to molecular biology techniques [7]. The use of mass spectrometry technology like MALDI-TOF MS is acquiring an increasingly important role in identifying and detecting these microorganisms [8]. This technology requires neither extensive training nor cost and it has been reported that it provides identification to genus and species level with an accuracy that approaches that of genetic methods.
Antimicrobial susceptibility
It is essential to test the antimicrobial susceptibility in all clinically relevant isolates due to the variable susceptibility of these microorganisms. Overall, non-diphtheriae Corynebacterium species are constitutively resistant to macrolides, lincosamides and type B streptogramins; susceptible to cefotaxime, amoxicillin/clavulanate, rifampin, and vancomycin (the recommended drug to treat severe infections) and have variable susceptibility to other antibiotics. C. striatum is the species which exhibits the highest resistance pattern.
According to CLSI (Clinical and laboratory Standard Institute) guidelines the reference method is the broth microdilution technique. This committee provides interpretive criteria for penicillin and erythromycin based on minimum inhibitory concentration (MIC) values following testing by this method, and for cephalosporin and linezolid the criteria are currently adapted from those from Streptoccocus and Enteroccocus, respectively, and remaining criteria are adapted from those from Staphyloccocus.
Although some laboratories use the disc diffusion method for susceptibility testing, the interpretative categories for zone diameters need to be established. The diffusion gradient tests (i.e. Etest) showed a good correlation of MICs with the broth microdilution method.
Conclusion and future perspectives
It is clear that due to the increasing number of immunocompromised patients and those with pre-existing pulmonary diseases, non-diphtheriae Corynebacterium species should be considered as an emerging cause of lower respiratory tract infection. A rapid and accurate laboratory detection, identification and assessment of these opportunistic microorganisms are critical for the correct diagnosis, taking into consideration that some of them are resistant to multiple antibiotics. Although more studies are need to enhance the understanding of the clinical significance of these microorganisms, clinicians should be aware of the potential pathogenic role of these species in the context of immunosuppression or chronic respiratory disease and they should not be always considered as mere colonizers.
References
1. Díez-Aguilar M, Ruiz-Garbajosa P, Fernández-Olmos A, Guisado P, Del Campo R, Quereda C, Cantón R, Meseguer MA. Non-diphtheriae Corynebacterium species: an emerging respiratory pathogen. Eur J Clin Microbiol Infect Dis 2012; doi: 10.1007/s10096-012-1805-5.
2. Nhan TX, Parienti JJ, Badiou G, Leclercq R, Cattoir V. Microbiological investigation and clinical significance of Corynebacterium spp. in respiratory specimens. Diagn Microbiol Infect Dis 2012; 74(3): 236–241.
3. Otsuka Y, Ohkusu K, Kawamura Y, Baba S, Ezaki T, Kimura S. Emergence of multidrug-resistant Corynebacterium striatum as a nosocomial pathogen in long-term hospitalized patients with underlying diseases. Diagn Microbiol Infect Dis 2006; 54(2): 109–114.
4. Renom F, Garau M, Rubí M, Ramis F, Galmés A, Soriano JB. Nosocomial outbreak of Corynebacterium striatum infection in patients with chronic obstructive pulmonary disease. J Clin Microbiol 2007; 45(6): 2064–2067.
5. Souza MC, Santos LS, Gomes DL, Sabbadini PS, Santos CS, Camello TC, Asad LM, Rosa AC, Nagao PE, Hirata Júnior R, Guaraldi AL. Aggregative adherent strains of Corynebacterium pseudodiphtheriticum enter and survive within HEp-2 epithelial cells. Mem Inst Oswaldo Cruz 2012;107(4): 486–93.
6. Funke G, von Graevenitz A, Clarridge JE 3rd, Bernard KA. Clinical microbiology of coryneform bacteria.Clin Microbiol Rev 1997; 10(1): 125–159.
7. Bernard K. The genus corynebacterium and other medically relevant coryneform-like bacteria. J Clin Microbiol. 2012; 50(10): 3152–3158.
8. Gomila M, Renom F, Gallegos Mdel C, Garau M, Guerrero D, Soriano JB, Lalucat J. Identification and diversity of multiresistant Corynebacterium striatum clinical isolates by MALDI-TOF mass spectrometry and by a multigene sequencing approach. BMC Microbiol 2012;12: 52.
The authors
María Díez-Aguilar* MD; Rafael Cantón MD, PhD; and María Antonia Meseguer MD, PhD
Department of Clinical Microbiology, Ramón y Cajal University Hospital, Madrid, Spain
*Corresponding author
E-mail: maria_diez_aguilar@hotmail.com