Role of TSH receptor antibodies in the diagnosis of Graves’ disease
Hyperthyroidism can result from a number of different disorders including Graves’ disease. The diagnostic gold standard is based on radiological tests but measurement of thyroid stimulating hormone receptor antibodies plays an important role in the diagnosis of Graves’. It is important to understand the diagnostic strengths and limitations of these measurements.
by Dr Christopher Boot
Introduction
Hyperthyroidism is relatively common, with a prevalence of between 0.5 and 2 % [1]. A range of symptoms and signs are associated with hyperthyroidism because of the influence of thyroid hormones on multiple organ systems. Many of the most important manifestations are related to effects on the cardiovascular system, which may include tachycardia and arrhythmias. Untreated, hyperthyroidism is associated with significant morbidity and mortality. Hyperthyroidism can usually be diagnosed through the measurement of thyroid stimulating hormone (TSH) and free thyroxine (FT4), with TSH usually suppressed and FT4 raised [occasionally free triiodothyronine (FT3) is raised in the absence of elevated FT4].
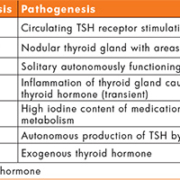
The major causes of hyperthyroidism are Graves’ disease and toxic multinodular goitre. Other etiologies include solitary toxic adenoma and thyroiditis (Table 1). Graves’ disease is the most common cause of hyperthyroidism with most other cases due to either toxic multinodular goitre or solitary toxic nodules, which result from autonomous secretion of thyroid hormones (T4 and T3) by one or more nodules. Transient thyrotoxicosis can occur as the result of thyroiditis, secondary to viral infection or autoimmunity.
Graves’ disease is an autoimmune disease characterized by stimulation of the thyroid by TSH receptor stimulating antibodies (TRAbs). This leads to the clinical features typical of hyperthyroidism such as weight loss, heat intolerance, palpitations, anxiety, tremor and tiredness. These autoantibodies may also recognize antigens in other tissues, notably fibroblasts in the eye muscles. This can lead to growth and inflammation of fat cells and muscles around the eye leading to Graves’ orbitopathy, characterized by upper eyelid retraction, lid lag, swelling, conjunctivitis and exophthalmos.
It is important to differentiate between Graves’ disease and other causes of hyperthyroidism as the approach to treatment may depend on etiology. Current guidelines recommend that all cases of hyperthyroidism are referred to an endocrinologist for further investigation to determine the cause and a treatment plan [2, 3]. This article focuses on the role of TRAb measurements in the diagnosis of Graves’ although TRAbs also provide prognostic information [4] and have a role in assessing the risk of neonatal hyperthyroidism in pregnancies involving maternal Graves’ [5].
Diagnosis of Graves’ disease
Determining the underlying cause of hyperthyroidism relies on a combination of clinical history, physical examination, biochemical testing and imaging. Certain findings are highly suggestive of Graves’ disease such as a symmetrically enlarged, non-nodular thyroid and evidence of orbitopathy. The most commonly used imaging tests are radiolabel uptake scans, which allow visualization of a thyroid radiolabel uptake pattern. In Graves’ disease there is homogenous, increased uptake of label across the thyroid, whereas in multinodular goitre there is patchy uptake with increased uptake at the sites of the over-active nodules. Radioactive iodine has largely been replaced with technetium pertechnetate (99mTc), which mimics the behaviour of iodine but exposes patients to lower radiation doses. The recommended role for TRAbs in the diagnosis of Graves’ varies. One recommended approach is to measure TRAbs in new cases of primary hyperthyroidism and where TRAb results are positive to diagnose Graves’ disease (Fig. 1). Where TRAb results are negative, uptake scans can then be used to distinguish Graves’, toxic nodule(s) and thyroiditis [6]. However, some guidelines have recommended an uptake scan as the first-line test, with TRAbs only used in certain situations [7].
TRAb assays
There are two main categories of TRAb assays. The majority of assays in clinical use detect TRAbs in patient samples through their competition with an added TSH receptor ligand for binding of the TSH receptor. These competition-based assays are sometimes referred to as thyrotropin-binding inhibitory immunoglobulin (TBII) assays. Competition-based assays do not discriminate between stimulatory TRAbs (as found in Graves’) or non-stimulating (inhibiting or neutral) TRAbs. In cases of hyperthyroidism it is assumed that any detected TRAbs are stimulating. The second category of TRAb assay is bioassays, which detect only stimulating TRAbs.
Competition-based assays have evolved over the years. Early assays used porcine thyroid membrane extracts and detected the inhibition of binding of radiolabelled TSH to these extracts. Liquid-phase assays were developed when recombinant human TSH receptor became available and the inhibition of radiolabelled TSH to recombinant TSH receptor was detected. Further evolution of competition assays involved replacement of labelled TSH with monoclonal anti-TSH receptor antibodies as the competing ligand. Modern TRAb assays typically use fluorescent or chemiluminescent labels and can be automated allowing high throughput.
Bioassays for stimulating TRAbs detect the production of cAMP in cells incubated with patient serum. Current bioassays use Chinese hamster ovary (CHO) cells transfected with human TSH receptor. These cells produce cAMP in response to TSH receptor stimulation. cAMP can be measured by immunoassay or a luciferase reporter gene may be used to generate a chemiluminescent signal in response to increasing cAMP. TRAb bioassays are more complex and expensive than competition-based assays and less commonly used in clinical practice.
Diagnostic performance of TRAb assays
The current generation of competition-based TRAb assays are generally reported to offer a high degree of diagnostic specificity and sensitivity for Graves’ disease. A meta-analysis of clinical studies using current assays indicated a pooled specificity of 99 % and sensitivity of 97 % [8]. This high diagnostic performance has led some authors to recommend TRAbs as a first-line test to distinguish Graves’ disease from other causes of hyperthyroidism. This may lead to a quicker and more cost effective diagnosis in many cases compared to initial use of imaging tests [9]. In particular, the high diagnostic specificity achieved means that untreated, hyperthyroid patients with positive TRAbs are highly likely to have Graves’ disease so that uptake scans may not be necessary in this scenario, particularly when the clinical presentation suggests Graves’. However, a recent study that compared the diagnostic sensitivity of a number of competition-based TRAb assays found significant variability with sensitivity varying from 65 to 100 % depending on the TRAb assay used [10]. Therefore, a negative TRAb result may not always rule out Graves’ disease with a high degree of certainty.
Assessment of the diagnostic performance of TRAbs in a UK tertiary referral centre
In view of the variability in reported diagnostic sensitivity and the identification of a number of cases of apparent TRAb-negative Graves’ disease in our centre, a retrospective study of the performance of TRAbs in the diagnosis of Graves’ was carried out. The Kryptor (ThermoFisher) TRAb assay was used throughout the period of the study. Results from all TRAb requests for patients referred with a new presentation of thyrotoxicosis were gathered over 18 months. Routine diagnosis of the etiology of hyperthyroidism was based on the uptake pattern on 99mTc scintigraphy, clinical course and other features in addition to TRAb concentrations. Ninety-nine cases of Grave’s disease were identified and 131 cases where an alternative cause of thyrotoxicosis was diagnosed. There was some overlap in TRAb concentrations between patients with Graves’ and patients with other etiologies (Fig. 2). Using the diagnostic cut-off of >1.8 IU/L suggested by the manufacturers of the assay, diagnostic sensitivity was 81.8 % (18 of 99 cases of Grave’s were TRAb-negative), whereas diagnostic specificity was 99.2 %. Applying a lower cut-off of >1.2 IU/L resulted in an improved sensitivity of 88.9 % but slightly lower specificity of 97.7 %.
This data from our centre demonstrated a significant number of cases of TRAb-negative Graves’ disease among patients referred with a new presentation of thyrotoxicosis. The diagnostic sensitivity of the Kryptor TRAb assay, therefore, appears to be lower than that suggested by the manufacturer’s data (96.3 %). This could possibly be as a result of more stringent classification of Graves’ in other studies, whereas this data represents the range of patients investigated in practice, which includes cases of borderline/mild hyperthyroidism. Of the 99 cases of Graves’ disease in this study, 40 patients had a FT4 of less than 30 pmol/L. Twenty percent of patients in this group had a TRAb level of <1.0 IU/L (the lower limit of quantification for the assay). Of the remaining 59 cases of Graves’ disease with a FT4 of ≥30 pmol/L, only 5 % had a TRAb level of < 1.0 IU/L. This suggests that cases of Graves’ with milder biochemical thyrotoxicosis on presentation are more likely to be TRAb-negative. Applying a lower diagnostic cut-off than that recommended by the manufacturer may improve the sensitivity of the Kryptor TRAb assay in the diagnosis of Grave’s disease. Practice in our laboratory is now to report an ‘equivocal’ range of 1.0–1.8 IU/L in addition to a cut-off for positivity of >1.8 IU/L. This better reflects the overlap in TRAb concentrations between Graves’ and other causes of thyrotoxicosis observed in our study than a binary positive/negative threshold. However, no cut-off provided 100 % diagnostic sensitivity for Graves’ disease.
Summary
TRAb assays are useful in the differentiation of Graves’ disease from other causes of thyrotoxicosis. In particular, TRAbs appear to provide a high degree of diagnostic specificity so that hyperthyroid patients with positive TRAb results are highly likely to have Graves’. Radioactive uptake scans may, therefore, not be necessary in all cases of TRAb-positive hyperthyroidism. However, some studies (including our local data) suggest that the diagnostic sensitivity of a negative TRAb result alone is not sufficient to reliably rule out Graves’ disease. Diagnostic performance is likely to vary between TRAb assays, so assay-specific reference data should be used for interpretation.
References
1. Vanderpump MPJ. The epidemiology of thyroid disease. Br Med Bull. 2011; 99: 39–51.
2. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, Rivkees SA, Samuels M, Sosa JA, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016; 26: 1343–1421.
3. UK Guidelines for the use of thyroid function tests. Association of Clinical Biochemistry, British Thyroid Association and British Thyroid Foundation 2006.
4. Vos XG, Endert E, Zwinderman AH, Tijssen JG, Wiersinga WM. Predicting the risk of recurrence before the start of antithyroid drug therapy in patients with Graves’ hyperthyroidism. J Clin Endocrinol Metab. 2016; 101(4):1381–1389.
5. Laurberg P, Nygaard B, Glinoer D, Grussendorf M, Orgiazzi J. Guidelines for TSH-receptor antibody measurements in pregnancy: results of an evidence-based symposium organized by the European Thyroid Association. Eur J Endocrinol. 1998; 139: 584–586.
6. Vaidya B, Pearce SHS. Diagnosis and management of thyrotoxicosis. BMJ 2014; 349: g5128.
7. Bahn RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, Laurberg P, McDougall IR, Montori VM, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association of Clinical Endocrinologists. Endocr Pract 2011; 17: 457–520.
8. Tozzoli R, Bagnasco M, Giavarina D, Bizzaro N. TSH receptor autoantibody immunoassay in patients with Graves’ disease: improvement of diagnostic accuracy over different generations of methods. Systematic review and meta-analysis. Autoimmun Rev. 2012; 12: 107–113.
9. McKee A, Peryerl F. TSI assay utilization: impact on costs of Graves’ hyperthyroidism diagnosis. Am J Manag Care 2012; 18: e1–14.
10. Diana T, Wüster C, Kanitz M, Kahaly GJ. Highly variable sensitivity of five binding and two bio-assays for TSH-receptor antibodies. J Endocrinol Invest. 2016; 39: 1159–1165.
The author
Christopher Boot PhD, FRCPath
Department of Blood Sciences, Royal
Victoria Infirmary, Newcastle upon Tyne Hospitals NHS Foundation Trust,
Newcastle upon Tyne, UK
*Corresponding author
E-mail: christopher.boot@nuth.nhs.uk