Strategies to facilitate diagnosis of allergic patients using recombinant allergens
An increasing number of allergenic molecules are on the market for the goal of improving the diagnostic profile. These molecules give more information about poly-sensitizations, the distinction between co-sensitization or co-reactivity, and help to assess the potential severity of a clinical reaction, as some allergenic molecules can be ‘more dangerous’ than others. The commercially available molecules have a decision-making role within the framework of allergic immunotherapy (AIT) support and monitoring of immunological response during treatment.
by Dr F. Barocci, Dr M. De Amici, Dr S. Caimmi and Prof. G. L. Marseglia
Heterogeneity of ‘allergens’
A recombinant allergen is an allergenic molecule produced using biotechnology techniques originally identified from an allergenic extract. Recombinant allergens are produced without the proteins undergoing biological or genetic variation. This ensures consistent allergen quality, high standardization and identification of the allergenic profile of each patient, termed component resolved diagnosis (CRD) [1].
Recombinant DNA technology currently offers the possibility of producing well-defined and characterized allergens. It offers prospects of great interest from the point of view of both ‘diagnostic’ and ‘therapeutic’ avenues. The advent of recombinant allergen molecules provided new opportunities as the allergens can be produced in unlimited quantities, and innovative production techniques solve the problems concerning the cross-reactivity of IgE antibodies. Many different allergens from many different sources stimulate allergic responses from our immune system, and hence allergy diagnosis is evolving with the use of new technologies such as nanotechnologies, molecular biology, to determine ‘cross-reactivity’ and ‘co-sensitization’ [2].
Molecular-based allergy diagnostics represents a useful tool to distinguish genuine sensitizations from cross-reactions in poly-sensitized patients, where traditional diagnostic tests and clinical history are unable to identify the relevant allergens for allergen immunotherapy (AIT) [3].
AIT in an expensive treatment, typically used over longer periods of time (3 to 5 years) and correct diagnosis, selection of truly eligible patients, identification of the primary sensitizing allergen are important for optimal and cost-effective patient management.
In fact, the patient may present various positivities giving rise to a ‘poly-sensitization’, which can be differentiated into:
- ‘co-sensitization’, presence of IgE reactivity directed to distinct and structurally unrelated epitopes
- ‘co-reactivity’ (cross-reactivity), presence of IgE reactivity where IgE antibodies raised against one allergen then bind homologous molecules in a different allergen.
Allergenic molecules can be:
- ‘genuine’, specific species found exclusively in a source (food or other), indicate a real sensitization (e.g. pollen)
- ‘pan-allergens’, present in different, unrelated sources (food and non-food), indicate cross-reactivity (e.g. between food and pollen) [4].
Examples of pan-allergens are the polcalcins, allergenic calcium-binding proteins (CBPs) present in pollen of all plant species; the profilins, cytoskeletal proteins of plants present in all pollen, but also in foods of plant origin; the lipid transfer protein (LTP), present in many plant foods (particularly those in the Rosaceae family); and cross-reactive carbohydrate determinants (CCD), found in pollen, plant foods, insects and venom.
Characteristics of allergenic proteins
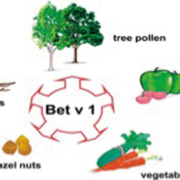
Allergenic proteins belong to both the Plant kingdom and the Animal kingdom, perform functions as varied as metabolic enzyme activities, structural or storage roles, some are glycosylated and some are similar structurally based on the biological relationship. The most studied and the most common allergenic molecules in the plant world are the families of proteins PR-10 (pathogenesis-related protein), known as Bet v 1 homologous proteins; the non-specific lipid transfer protein (nsLTP); profilin, also termed Bet v 2, and homologous proteins (2S albumin, 7S/11S globulin).
The vast majority (90–98%) of patients allergic to birch (family Betulaceae, order Fagales) test positive for IgE to
Bet v 1 proteins, which are thermolabile and modified during digestion [5].
The Bet v 1 specific IgE antibodies cross-react with Bet v 1 homologues present in pollen of plants included such as hazel, alder and hornbeam (family Fagaceae, order Fagales) [6] and in foods of plant origin such as apple, carrot, celery, cherry and pear. The clinical manifestations are related to the oral allergy syndrome (OAS)-type clinical reactions localized in the oral cavity and patients allergic to protein Bet v 1 homologous frequently reported good tolerance for cooked foods and commercial fruit juices.
Allergenic molecules including the birch-related profilins, or Bet v 2, are recognized in 10–20% of patients allergic to trees, grasses, herbs, fruits, vegetables, nuts, spices and latex. The Bet v 4 or calcium binding protein (CBP) allergens are present in pollen (grasses, trees, and herbs). Pollen germination occurs in the presence of calcium ions and is under the control of a class of CBPs that are found only in mature pollen. Patients who produce IgE to CBP are allergic patients or are at risk of developing allergic symptoms after contact with pollen. However, these allergens are not involved in food-plant-derived allergies.
Molecular allergens are grouped into different families depending on their molecular conformation and can provoke clinical responses of lesser (oral allergy syndrome), or greater (systemic allergic reactions) severity. The proteins PR-10 and the profilins generally are sensitive to heat and protease, so the clinical expression is related primarily to the OAS-type events. The nsLTPs and the storage proteins are not sensitive to heat or gastric digestion, and so can cause systemic reactions; however, patients allergic to LTP frequently have a good tolerance to peeled fruit [7]. Plant-based foods are a major cause of allergy and sensitivity in populations of southern Europe (Italy and Spain).
The nsLTPs are present in the Rosaceae (e.g. Pru p 3), and are also in walnut, hazelnut, corn, sesame seeds, sunflower seeds, beer, grapes, peanuts, mustard (e.g. Cor 8) [8]. The presence of LTPs in tomatoes has been highlighted, because even with peeled tomatoes, there are other LTP isoforms in the pulp and seeds [9].
The family of ‘storage proteins’ are a heterogeneous group of proteins that belong to two different superfamilies: cupins (e.g. 7/8S and 11S globulins) and prolamins (e.g. 2S albumin). The presence of IgEs against storage proteins is considered as an important marker of severe systemic reactions, for example as in allergy to peanuts (Ara h 2, Ara h 3), cereals, walnut, hazelnut, sesame, etc. These proteins are highly resistant to heat and peptic digestion and also cause sensitization in both the gastrointestinal and respiratory tracts. The substantial difference between foods of plant origin and foods of animal origin is that plant-derived foods contain both stable and labile allergenic proteins; whereas those of animal origin are mostly characterized by allergenic proteins resistant to heat and digestion [10].
The ‘opportunity’ approach
Molecular-based allergy diagnostics has emerged into routine care due to its ability to improve risk assessment, particularly for food allergies. Different foods contain unique allergenic molecules that are stable or labile to heat and digestion. The stability of a molecule and a patient’s clinical history help the clinician evaluate the risk of systemic versus local reactions. Labile allergens are linked to local reactions (typically oral symptoms) and cooked food is often tolerated, whereas stable allergens tend to be associated with systemic reactions in addition to local reactions [11].
Here, we discuss some of the most commonly used recombinant molecules for evaluating allergic patients [12].
Egg albumin
The most common of the food allergies of animal origin described here is that of egg albumen sensitivity. In this case at least two more allergens should be tested: Ovomucoid (Gal d 1) and Ovalbumin (Gal d 2) [13]. Ovomucoid is resistant to heat, urea and digestive proteases and, therefore, can trigger severe allergic reactions when the egg is ingested raw or cooked. Ovalbumin is thermo-stable, thus loses part of its allergenicity after heat treatment, and is also digested by peptidases. Ovalbumin has, then, generally lower allergenicity than ovomucoid, causing less severe allergic reactions, although occasionally exceptionally severe reactions to flu vaccines have been noted. The development of tolerance to the major molecular components of eggs is achieved normally within 4 years for ovalbumin, although not normally reached for ovomucoid. In addition, it is important to test for a reaction to egg-white lysozyme. This so-called ‘hidden’ allergen is frequently used in food preparation as a preservative and additive (e.g. in hard cheese), to prevent the formation of bacterial colonies and poses a risk to patients because it is not normally listed on food ingredient labels.
Milk
Milk contains more than 40 proteins, all of which may act as antigens for humans. Beta-lactoglobulin (BLG) and alpha-lactoalbumin (ALA) are the main proteins that are synthesized from the mammary gland, causing moderate reactions; essentially they are sensitive to heat and usually tolerance develops within 4 years. The milk of various ruminants from buffalo to cow, sheep and goat contains the same or very similar proteins that share structural and functional characteristics. Human milk contains no BLG, and the most concentrated protein is ALA, which is important in the nutrition of the newborn. Human and bovine milk differ substantially in the proportion of serum protein casein present; approximately 60 : 40 in human milk and about 20 : 80 in bovine milk and in the proportion of specific proteins. Casein is found in milk and dairy products, especially cheese, and is also often used in other foods such as sausages, soups, etc., often as a hidden ingredient. It can cause severe reactions as it is not heat labile and so tolerance does not normally develop [14].
Soybeans
One of the most important vegetables that causes allergy is soybeans. These are either used fresh or as flour, flakes, soy milk or processed to collect the oil, which is a cause of occupational asthma and is used for pharmaceuticals, cosmetics and other industrial applications. The soy allergy prevalence is estimated at 0.4% in the general population, is found in 6% of atopic children and in 14% of patients who are allergic to milk. The greatest difficulty in making a diagnosis of true soy allergy is in the differentiation of cross-reactivity with birch and peanuts [15, 16].
Shrimp
The major allergen of shrimp is tropomyosin, Pen a 1, positive in 80% of patients allergic to shellfish. It is present in muscle tissues of all living beings and therefore has a strong homology in crustaceans and shellfish (shrimp, prawns, lobster, crab, oysters, snails, squid) justifying a cross-reactivity between different species. Shrimp tropomyosin also has a high structural identity to the tropomyosin in other invertebrates, such as mites and cockroaches [17]. Patients allergic to dust mites and cockroaches will also have reactivity towards Pen a 1 without having come into contact with shellfish. Targeted immunotherapy for mite allergy can induce allergic reactions to shrimp or snails. Hence, when such therapeutic approaches are used for mite allergy, there is always the risk of causing food sensitisation in the patient.
Conclusion
Diagnostic molecular allergology is valid for discriminating allergic patients; differentiating true ‘allergies’ from ‘cross-reactivity’; leading to a more accurate ‘diagnosis’ and so reducing the need for oral food challenges; and predicting ‘severe reactions’ and ‘persistence of allergy’. Molecular diagnostics must be used for ‘targeted’ lead to a correct evaluation, and to reduce the use of oral challenges.
When a food allergen is suspected of causing allergic-type reactions of greater or lesser severity the various components of cross reactions associated with food/pollens and cross reactions between foods must be taken into account. Therefore, allergy diagnostics in vitro has often traditionally looked like positivity among individual patients giving seemingly similar laboratory results, but only the use of molecular diagnostics can draw out and highlight the differences in laboratory data in order to have a detailed specificity for various allergenic components, and then a differential clinical significance. Hence, the real situation of the patient can be defined. In order to provide the correct therapy, it is essential to know if the patient has a ‘true allergic’ reaction to the molecules specific to a particular species or if the patient has many positive results because of structural homology between different proteins.
The request for specific IgE assays should always start from a clinical evaluation and an earlier investigation in vivo or in vitro, using allergenic extracts.
References
1. Maiello N. [Allergy diagnosis: component resolved diagnosis.] Società Italiana di Immunologia e Allergologia Pediatrica, www.siaip.it (in Italian).
2. Ballmer-Weber BK, Scheurer S, Fritsche P, Enrique E, Cistero-Bahima A, Haase T, Wüthrich B. Component-resolved diagnosis with recombinant allergens in patients with cherry allergy. J Allergy Clin Immunol. 2002; 110: 167–173.
3. Alberse RC. Assessment of allergen cross-reactivity. Clin Mol Allergy 2007; 5: doi: 10.1186/1476-7961-5-2.
4. Ledesma A, Barderas R, Westritschnig K, Quiralte J, Pascual CY, Valenta R, Villalba M, Rodríguez R. A comparative analysis of the cross-reactivity in the polcalcin family including Syr v 3, a new member from lilac pollen. Allergy 2006; 61: 477–484.
5. Jarolim E, Rumpold H, Endler AT, Ebner H, Breitenbach M, Scheiner O, Kraft D. IgE and IgG antibodies of patients with allergy to birch pollen as tools to define the allergen profile of Betula verrucosa. Allergy 1989; 44: 385–395.
6. Mari A, Wallner M, Ferreira F. Fagales pollen sensitization in a birch-free area: a respiratory cohort survey using Fagales pollen extracts and birch recombinant allergens (rBet v 1, rBet v 2, rBet v 4). Clin Exp Allergy 2003; 33: 1419–1428.
7. Asero R, Mistrello G, Roncarolo D, Amato S, Zanoni D, Barocci F, Caldironi G. Detection of clinical markers of sensitization to profilin in patients allergic to plant-derived foods. Allergy Clin. Immunol. 2003; 12(2): 427–432.
8. Fernández-Rivas M1, González-Mancebo E, Rodríguez-Pérez R, Benito C, Sánchez-Monge R, Salcedo G, Alonso MD, Rosado A, Tejedor MA, Vila C, Casas ML. Clinically relevant peach allergy is related to peach lipid transfer protein, Pru p 3, in the Spanish population. J Allergy Clin Immunol. 2003; 112: 789–795.
9. Asero R, Mistrello G, Roncarolo D, Amato S, Caldironi G, Barocci F, Van Ree R. Immunological cross-reactivity between lipid transfer proteins from botanically unrelated plant-derived foods: a clinical study. Allergy 2002; 57(10): 900-906.
10. Van Zuuren EJ Terreehorst I, Tupker RA, Tupker RA, Hiemstra PS, Akkerdaas JH. Anaphylaxis after consuming soy products in patients with birch pollinosis. Allergy 2010; 65(10): 1348–1349.
11. Macchia D, Capretti S, Cecchi L, Colombo G, Di lorenzo G, Fassio F. Position statement: in vivo and in vitro diagnosis of food allergy in adults. It J Allergy Clin Immunol. 2011; 21: 57–72.
12. Huang F, Nowak-Węgrzyn A. Extensively heated milk and egg as oral immunotherapy. Curr Opin Allergy Clin Immunol. 2012; 12(3): 283–292.
13. Vazquez-Ortiz M, Alvaro M, Piquer M, Dominguez O, Machinena A, Martín-Mateos MA, Plaza AM. Baseline specific IgE levels are useful to predict safety of oral immunotherapy in egg-allergic children. Clin Exp Allergy 2014; 44(1): 130–141.
14. Caubet JC, Nowak-Węgrzyn A, Moshier E, Godbold J, Wang J, Sampson HA. Utility of casein-specific IgE levels in predicting reactivity to baked milk. J Allergy Clin Immunol. 2013; 131(1): 222–224.e4.
15. Kerre S. [Anaphylactic reaction to a soya dietary drink in a birch pollen allergic patient]. Revue Francaise d’Allergologie et d’Immunologie Clinique 2007; 47; 416–417 (in French).
16. Holzhauser T, Wackermann O, Ballmer-Weber BK, Bindslev-Jensen C, Scibilia J, Perono-Garoffo L, Utsumi S, Poulsen LK, Vieths S. Soybean (Glycine max) allergy in Europe: Gly m 5 (beta-conglycinin) and Gly m 6 (glycinin) are potential diagnostic markers for severe allergic reactions to soy. J Allergy Clin Immunol. 2009; 123: 452–458.
17. La Grutta S, Calvani M, Bergamini M, Pucci N, Asero R. [Tropomyosin allergy: from molecular diagnosis to the clinic.] Rivista di Immunologia e Allergologia Pediatrica 2011; 2: 20–38 (in Italian).
Acknowledgement
The Authors declare no conflict of interest.
Thanks go to Cristina Torre, Giorgia Testa, Sabrina Nigrisoli for their active cooperation at the Laboratory of Immuno-Allergology, Pediatric Clinic, IRCCS Foundation Polyclinic San Matteo, Italy.
Alberto G. Martelli and Giovanni Traina, Department of Paediatrics, S. Corona Hospital, Garbagnate Milanese, Italy, are also thanked for their collaboration.
The authors
Fiorella Barocci*¹ PhD, Mara De Amici² PhD, S. Caimmi² MD, G. L. Marseglia² MD
1Department of Immunohematology and Tranfusion medicine, “di Circolo” Hospital, Rho, A.O.G Salvini Garbagnate Milanese, Italy
2Department Clinica Pediatrica, Università degli Studi di Pavia, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy
*Corresponding author
E-mail: fiorellabarocci@yahoo.it