Targeted testing for HIV in hospital emergency departments has great potential, Spanish researchers say
-
Strategy led to number of HIV diagnoses increasing more than three-fold
-
Implemented country-wide, it would prevent 13,615 new infections and save €4,411 million in healthcare costs in two decades
Note: the release below is a special early release from the European Congress of Clinical Microbiology & Infectious Diseases (ECCMID 2023, Copenhagen, 15-18 April).
Targeted testing for HIV in emergency departments has great potential for increasing diagnoses,this year’s European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) in Copenhagen, Denmark, (15-18 April), will hear.
An analysis of data from 34 emergency departments (ED) in Spain found that the number of HIV diagnoses more than trebled after targeted testing was implemented.
Researcher Dr Juan González del Castillo, head of the Infectious Disease Group of Spanish Emergency Medicine Society (SEMES), says: “Early diagnosis is key to avoiding the spread of HIV infection and improving patients’ prognosis but rates of undiagnosed and late-diagnosed infections are still high.
“An estimated 20% of infected people globally do not know they are living with HIV and late diagnosis rates are close to 50% in the developed world. In Spain, the figure is 48%.
“Screening for HIV in hospital emergency departments could increase the number of diagnoses, as well as allow more cases to be detected earlier.”
Guidance released by SEMES in 20211,2 recommends the promotion of HIV testing and referral to appropriate specialists for follow-up in individuals attending emergency departments (ED) for treatment related to one of six conditions or behaviours: sexually transmitted infections (STI), mononucleosic syndrome (MN), herpes zoster virus (HZ), community-acquired pneumonia (CAP), practice of chemsex (CS) and HIV post-exposure prophylaxis (PEP). These are common in people with HIV and are also frequently seen in ED.
In this longitudinal study, Dr González del Castillo, head of the emergency department at Hospital Clínico San Carlos, Madrid, Spain, and colleagues used administrative data and medical charts from 34 Spanish EDs (13% of the national network) participating in theDejatuhuella (Leave your mark) programme to evaluate levels of HIV testing before (July-Dec 2019) and after (Jan to June 2022) the SEMES guidance was implemented.
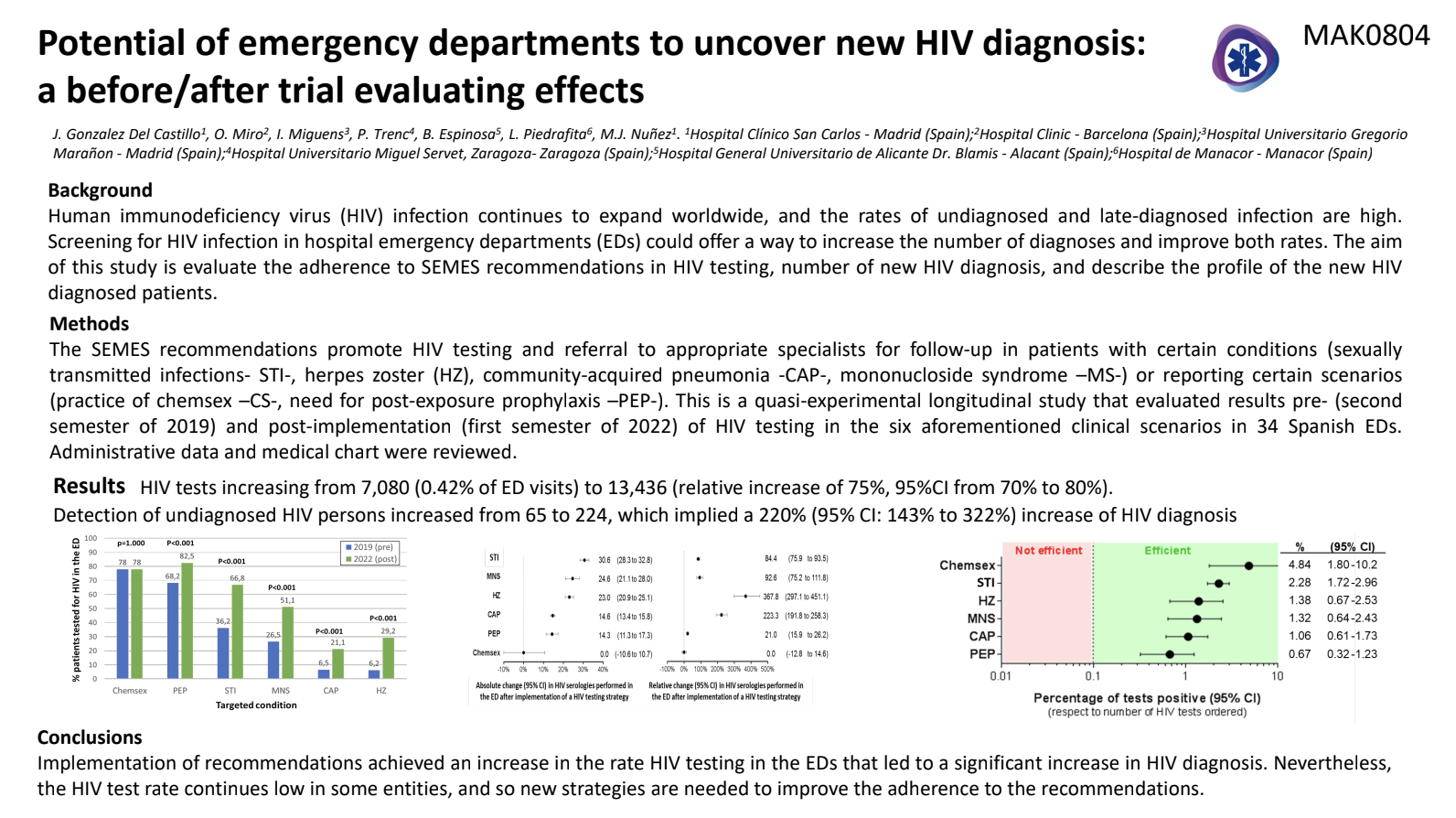
The number of HIV tests ordered in ED increased from 7,080 to 13,436. This represents an increase of 75%, when differences in the number of people attending ED are taken into account.
The number of HIV diagnoses increased more than three-fold, from 65 to 224. This represents an increase of 220%, when ED attendance figures are factored in.
The positive test rate increased from 0.92% to 1.67%. This was expected, as previous studies had shown a high positive rate in the six conditions and behaviours covered by the SEMES recommendations.
There was a significant increase in HIV testing in all of the recommended areas, apart from practice of chemsex. STI (36% of patients tested for HIV before implementation vs. 67% after implementation), MS (27% vs. 51%), CAP (7% vs. 21%), HZ (6% vs. 29%), PEP (68% vs 83%). The rate of HIV in CS remained unchanged at 78%.
The demographic and health characteristics of the individuals diagnosed in both periods were similar.
There was a significant reduction in the time between ED attendance and the first appointment with an HIV specialist (median of 30 days vs. 7 days), as well as the initiation of antiviral treatment (median of 24 days vs.14 days).
The study’s authors conclude that the implementation of targeted testing for HIV in emergency departments led to a significant increase in HIV diagnoses.
To date, a total of 103 EDs have implemented the recommendations. Data from SEMES shows that in 2021 and 2022, 113,030 tests were performed, with 287 HIV diagnoses in 2021 and 601 in 2022 –888 new diagnoses in these two years.3 (It isn’t possible to make comparison with earlier years.)
If it is assumed that one diagnosis prevents another two to four cases, the new diagnoses in these two years will have led to 1,756 to 3,512 new cases being avoided.3
Dr González del Castillo says: “We really hope that the Dejatuhuella programme will reverse the downward trend in HIV diagnoses in Spain and reduce the spread of HIV and the high rates of late diagnosis.
“EDs could play a crucial role in HIV diagnosis. We know from previous research that one in three missed opportunities to diagnose HIV occurs in ED and we also know that for many people, their ED is their only point of contact with the healthcare system.
“Increasing the rates of diagnosis and early diagnosis doesn’t just have huge implications for individuals’ health and public health, it would also be cost-effective.
“A recent economic assessment of the SEMES strategy4 calculated that it would prevent 13,615 new infections and have potential savings for the healthcare system of €4,411 million in two decades, with an economic return of €224 per euro invested.”
Targeted screening is one of the two main methods of HIV screening in ED; the other is opt-out screening.
A project in the England is using opt-out HIV testing in A&Es in areas with the highest prevalence of HIV. All adults who are having blood tests while in A&E are tested for HIV unless they opt out. In many areas, hepatitis B and hepatitis C are also tested for.
Data from the 28 A&Es participating in the first 100 days of the project (April to July 2022) shows that more than 250,000 HIV tests were carried out. There were 128 HIV diagnoses, 325 hepatitis B diagnoses and 153 hepatitis C diagnoses.5
“It would be difficult to implement a universal testing strategy like this in Spain, where explicit consent for HIV testing is required,” says Dr González del Castillo. “In addition, some ED physicians may be reluctant to order tests that will not help them diagnose and treat the condition that patient has presented with.
“Targeted HIV screening in the ED, as we are doing in Spain, can be impactful, more cost-effective, and better accepted by both patients and physicians than universal testing.
“On the other hand, we are working on recommendations for hepatitis B and C testing and many EDs have already started doing it at the same time as HIV, with 63 new hepatitis C diagnosis in 2021 and 2022.”
He concludes: “The role that ED can play in HIV detection is pivotal and must be recognised and promoted, whatever the strategy and wherever people are in the world.”