The role of lipid measurement in the assessment of cardiovascular disease risk: when to screen and what to measure
Cardiovascular disease (CVD) carries considerable morbidity and mortality and poses a large economic cost on societies. Screening for CVD in order to identify high-risk individuals who may then be treated has been shown to be an effective way of alleviating the associated burden of disease. Numerous risk factors have been identified, of which lipids are a major modifiable factor.
by Dr Ravinder Sodi, Jarlath Eastwood, Dr Ian M. Godber
Cardiovascular disease (CVD), which manifests as coronary artery disease, peripheral vascular disease and cerebrovascular disease, accounts for approximately one-third of deaths worldwide [1], with three-quarters of them occurring in middle- and low-income countries [2]. The assessment of risk factors helps to determine those who are at high risk for CVD, which may then lead to lifestyle and dietary modifications as well as the use of medications in an attempt to mitigate the risk of associated mortality and morbidity. The primary aim of lipid measurements in the clinical setting is to aid in cardiovascular disease risk estimation. In the United Kingdom (UK), the National Institute for Health and Care Excellence (NICE) has issued guidance on the cardiovascular risk assessment and the modification of blood lipids to prevent CVD [3].
Clinical indications for screening
The clinical indication for screening is to identify high-risk individuals for the primary (first event) prevention of CVD. The most recent NICE guidance [3] recommends screening all individuals aged 40–74 years and/or with type 2 diabetes mellitus (DM) using the QRISK2 screening tool [3]. If the 10-year risk is ≥20%, a full, formal risk assessment should be undertaken; otherwise reviewing on an ongoing basis is suggested. The guidelines state ‘offer atorvastatin 20 mg for the primary prevention of cardiovascular disease (CVD) to people who have a 10% or greater 10-year risk of developing CVD’ [3]. This recommendation has not yet been widely adopted and has been critiqued as it would mean that a considerable proportion of the general population would require lipid-lowering therapy [4]. If the 10-year risk is ≥20%, lifestyle changes as well as lipid-lowering medications should be considered. The use of clinical judgement and pragmatism is advised. The QRISK2 is not applicable in those ≥85 years; with type 1 DM; an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73m2, albuminuria or both; pre-existing CVD; and, family history of dyslipidemia. These patients are already at high risk and as such screening is of no further benefit. It is important to bear in mind that CVD risk may be underestimated in people treated for HIV, those with serious mental health issues, medications causing dyslipidemias, systemic inflammatory disorders, those on anti-hypertensives or lipid-lowering drugs, those who are severely obese (body mass index, BMI >40 kg/m2) and those who have recently stopped smoking. In general, for both primary and secondary prevention of CVD, the cardio-protective diet, physical activity, weight management, reduced alcohol consumption and smoking cessation are recommended together with lipid modification therapy, as applicable.
Risk factors for cardiovascular disease
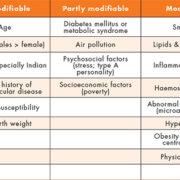
There are numerous modifiable, partly modifiable and unmodifiable risk factors for CVD as shown in Table 1 [5]. The major modifiable risk factors for CVD are cigarette smoking, hypertension, dyslipidemia and depending on the presence of chronic complications of hyperglycemia, DM may be a partly modifiable factor. CVD risk increases with age and is higher in males than females, with the exception of postmenopausal women who smoke [6]. CVD is more common in those with a family history of the same and appears to be more common in Indians compared to Caucasians [1, 7]. Partly modifiable risk factors may be difficult to modulate as these may be beyond the control of both patient and clinician.
Lipid variables and cardiovascular disease risk
An elevated plasma concentration of low-density lipoprotein (LDL)-cholesterol has been shown to be a strong independent predictor of CVD [8]. Lipid-lowering guidelines have recommended LDL-cholesterol as the main target of treatment with lipid-lowering drugs. Astonishingly, the Friedewald formula (Table 2) used to determine the LDL-cholesterol in most clinical laboratories [9] has never been validated for use in patients treated with lipid-lowering medications. This information is not always available to laboratories when reporting lipid results. Moreover, this formula is only valid in individuals with triglycerides <4.5 mmol/L, necessitating an overnight fast before its determination and is inaccurate in those with low LDL-concentrations. As there are three variables required to determine LDL-cholesterol using the Friedewald formula, it is subject to three sources of inherent bias and imprecision. It also assumes that the cholesterol content of the very-low density lipoprotein (VLDL)-cholesterol is constant and does not account for other atherogenic lipoproteins and, therefore, is not valid in those with familial dysbetalipoproteinemia (type III hyperlipoproteinemia, broad-beta disease or remnant removal disease) where the LDL-cholesterol is overestimated [10]. Finally, it must be pointed out that the recommended QRISK2 tool does not require LDL-cholesterol as a variable to determine CVD risk but requires total-cholesterol and high-density lipoprotein (HDL)-cholesterol as separate variables [11].
HDL-cholesterol is a powerful independent cardiovascular risk factor with an inverse relationship with atherosclerotic disease (with risk rising sharply when levels are <1.04 mmol/L) [12]. However, Total-cholesterol/HDL-cholesterol ratio has been shown to be a better measure of CVD risk than individual components [13]. Total-cholesterol and high-density lipoprotein (HDL)-cholesterol are included in the QRISK2 tool as separate entities in determining CVD risk [3, 11].
Non-HDL-cholesterol (Table 2) has long been known to be a better predictor of CVD risk than LDL-cholesterol, but is as good as apolipoprotein-B [14]. It is known that many patients who achieve their LDL-cholesterol targets still develop CVD due in part to the residual risk not identified by LDL-cholesterol. Non-HDL-cholesterol serves as an index of all atherogenic, apolipoprotein-B containing lipoproteins: LDL, VLDL, intermediate-density-lipoprotein (IDL), lipoprotein(a). Most important, from a pragmatic stance, it does not require patients to be fasted overnight and can be used in those with high triglycerides. In addition, the recent NICE guidelines endorse the use of non-HDL-cholesterol recommending specialist referral if it is >7.5 mmol/L. Non-HDL cholesterol is particularly of importance in DM, where LDL-cholesterol may not be raised but the risk of CVD is considerable. Moreover, it has been shown that in DM, non-HDL cholesterol is a stronger predictor of mortality from CVD than LDL-cholesterol [15]. The prediction of CVD in those on lipid-lowering therapy remains an important goal and non-HDL-cholesterol may help address this. One disadvantage of non-HDL-cholesterol is that the positive bias in HDL-cholesterol measurement seen in cases of hypertriglyceridemia may mitigate any benefits [16]. However, taken together, non-HDL cholesterol provides an accurate alternative to LDL-cholesterol and there is a compelling case to include it in the laboratory test repertoire especially given that no additional reagent is required other than a simple calculation.
Elevated triglycerides concentrations are also an independent risk factor for CVD although it is weaker than LDL-cholesterol [17]. A high triglyceride level is a component of the metabolic syndrome, which is associated with high risk of CVD. Severe hypertriglyceridemia also increases the risk of pancreatitis [18]. Secondary causes of hypertriglyceridemia include: alcohol excess, medication-related (thiazides, beta-blockers, estrogens, corticosteroids, antiretroviral protease inhibitors, immunosuppressants, antipsychotics), untreated DM, renal disease, liver disease, pregnancy and some autoimmune disorders [18].
Apolipoproteins-B, -A1, low-density lipoprotein particle number and size have all been advocated as markers of CVD risk but offer no advantage over routine lipid parameters discussed above, are expensive requiring additional reagents but may be useful in identifying patients with dysbetalipoproteinemia [19]. At present in the UK, they are only measured in specialist laboratories.
Conclusion
Lipid testing offers a simple and cost-effective mode of determining CVD risk. Clinical laboratories should make every effort to start reporting non-HDL-cholesterol as part of their lipid profiles. It requires no additional reagent other than software configurations for calculation, obviates the need for fasting and requires no knowledge of lipid-lowering medications.
References
1. Moran AE, Roth GA, Narula J, Mensah GA. 1990–2010 global cardiovascular disease atlas. Glob Heart. 2014; 9: 3–16.
2. World Health Organization. Cardiovascular diseases (CVDs). WHO 2015; http://www.who.int/mediacentre/factsheets/fs317/en/
3. National Institute for Health and Care Excellence. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. Clinical Guideline 181. 2014; https://www.nice.org.uk/guidance/cg181.
4. Wise J. Open letter raises concerns about NICE guidance on statins. BMJ 2014; 348: g3937.
5. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364: 937–952.
6. Billups KL, Miner MM, Wierzbicki AS, Jackson G. Gender-based cardiometabolic risk evaluation in minority and non-minority men grading the evidence of non-traditional determinants of cardiovascular risk. Int J Clin Pract. 2011; 65: 134–147.
7. Lovegrove JA. CVD risk in South Asians: the importance of defining adiposity and influence of dietary polyunsaturated fat. Proc Nutr Soc. 2007; 66: 286–298.
8. McQueen MJ, Hawken S, Wang X, Ounpuu S, Sniderman A, Probstfield J, et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet. 2008; 372: 224–233.
9. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18: 499–502.
10. Zhao SP, Smelt AH, Leuven JA, van den Maagdenberg AM, van der Laarse A, van ‘t Hooft FM. Lipoproteins in familial dysbetalipoproteinemia. Variation of serum cholesterol level associated with VLDL concentration. Arterioscler Thromb. 1993; 13: 316–323.
11. Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008; 336: 1475–1482.
12. Cooney MT, Dudina A, De Bacquer D, Wilhelmsen L, Sans S, Menotti A, et al. HDL cholesterol protects against cardiovascular disease in both genders, at all ages and at all levels of risk. Atherosclerosis 2009; 206: 611–616.
13. Lemieux I, Lamarche B, Couillard C, Pascot A, Cantin B, Bergeron J, et al. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men: the Quebec Cardiovascular Study. Arch Intern Med. 2001; 161: 2685–2692.
14. Hirsch G, Vaid N, Blumenthal RS. Perspectives: The significance of measuring non-HDL-cholesterol. Prev Cardiol. 2002; 5: 156–159.
15. Liu J, Sempos C, Donahue RP, Dorn J, Trevisan M, Grundy SM. Joint distribution of non-HDL and LDL cholesterol and coronary heart disease risk prediction among individuals with and without diabetes. Diabetes Care 2005; 28: 1916–1921.
16. Cramb R, French J, Mackness M, Neely RD, Caslake M, MacKenzie F. Lipid external quality assessment: commutability between external quality assessment and clinical specimens. Ann Clin Biochem. 2008; 45: 260–265.
17. Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet 2014; 384: 626–635.
18. Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Sacks F, Murad MH, et al. Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012; 97: 2969–8299.
19. Dominiczak MH, Caslake MJ. Apolipoproteins: metabolic role and clinical biochemistry applications. Ann Clin Biochem. 2011; 48: 498–515.
The authors
Ravinder Sodi* 1,2 PhD, CSci, FRCPath; Jarlath Eastwood1 BSc, Ian M. Godber2 PhD, CSci, FRCPath
1Institute of Cardiovascular and Medical Sciences, University of Glasgow, Glasgow, UK
2Department of Clinical Biochemistry, NHS Lanarkshire, Wishaw General
Hospital, Wishaw, UK
*Corresponding author
E-mail: ravsodi@yahoo.com