Visual detection of Ebola virus: targeting the NP gene by RT-LAMP
Ebola virus (EBOV) can lead to severe hemorrhagic fever with a high risk of death in humans and other primates. More recently, reverse transcription loop-mediated isothermal amplification (RT-LAMP) has become readily available for the diagnosis of EBOV, and is a suitable tool for clinical screening, diagnosis and primary quarantine purposes.
by H. Li, W. Lin, X. Wang, X. Wei, E. Li, P. Li, J. Chen, S. Qi, Y. Ma, L. Cui, X. Hu, Dr X. Zhao, Prof. J. Yuan
The 2014 Ebola virus (EBOV; one of the world’s most virulent viruses) caused an outbreak of human disease with widespread transmission in multiple West African countries and sporadic cases in Europe and North America [1, 2]. The numbers of people infected and deaths were the most severe in history. However, the massive public health response has been limited, in part, by the inability to rapidly detect the presence of EBOV in potential patients living in remote areas [3].
EBOV, (species Zaire ebolavirus from the family Filoviridae), was first identified in Zaire in 1976 and named after the River Ebola in Zaire [4]. However, EBOV could not be detected rapidly in many potential patients living in remote and developing areas. The EBOV genome is approximately 19 kb, and encodes the seven proteins in the following order from the 3’-UTR: nucleoprotein (NP), viral structural protein (VSP)35, VSP40, glycoprotein (GP), VP30, VP24, and RNA-dependent RNA polymerase (L) [5]. As the NP gene is highly conserved among EBOV species, it is, therefore, recommended by the World Health Organization (WHO) for use as a target gene for the reverse transcription (RT)-PCR assay. The initial symptoms of EBOV infection could be confused with those of other febrile illnesses such as endemic malaria [6].
Current approaches for the laboratory diagnosis of EBOV infection include virus isolation, electron microscopy, immunohistochemistry, antigen-capture ELISA testing, IgM ELISA, RT-PCR, and serologic testing for IgM or IgG virus-specific antibodies. In 2015, Baca et al. presented a rapid detection of EBOV with a reagent-free, point-of-care biosensor. In general, the detection of EBOV antigens by antigen-capture ELISA is suitable as a method of laboratory diagnosis when the viral load in the blood reaches a very much higher case fatality rate. Thus, real-time (q)RT-PCR has taken over as a first choice diagnostic technique for detection of EBOV recommended by WHO [3]. However, Taq DNA polymerase in PCR-based techniques can be inactivated by inhibitors present in crude biological samples. Moreover, these methods are relatively complex and require specialized high-cost instruments.
Loop-mediated isothermal amplification (LAMP) is a one-step nucleic acid detection method developed by Notomi et al., which relies on autocycling strand displacement DNA synthesis [7]. This novel method is highly specific and sensitive, takes advantage of four or six specific primers to recognize six or eight different sequences of the target gene, and is performed under isothermal conditions in less than 1 h using Bst DNA polymerase. Kurosaki et al. developed a simple reverse transcription (RT)-LAMP assay for the detection of EBOV, targeting the trailer region of the viral genome. However, this method has yet to be tested in clinical samples [8].
To develop an RT-LAMP for clinical screening and rapid diagnosis of EBOV, we first selected potential target regions based on the NP sequences of the EBOV variant Mayinga (GenBank Accession no. AF086833), which were further analysed with Primer Explorer V4 software (http:/primerexplorer.jp/lamp) and subsequently the sequences were aligned with other species of EBOV. A total of five sets of primers were initially designed to detect artificially synthesized EBOV RNA using a real-time turbidimeter. To compare the sensitivity and specificity of RT-LAMP, normal RT-PCR was performed with the primers.
The RT-LAMP reactions were carried out in a 25-μl reaction mixture with an RNA amplification kit (Eiken Chemical Co. Ltd), in accordance with the manufacturer’s protocol. The reaction mixture contained the following reagents (final concentration): RT-LAMP mixture and 8 U Bst DNA polymerase. The amount of primer needed for one reaction was 80 pmol of forward and backward inner primers (FIP and BIP), 40 pmol of loop primer (LB), and 10 pmol of outer forward primer (F3) and outer backward primer (B3). Finally, an appropriate amount of genomic template DNA was added to the reaction tube. The reaction was carried out in the reaction tube at 61 °C, 60–80 min, in dry bath incubators.
Two different methods were used to detect RT-LAMP products. For direct visual inspection, 1 μl of calcein (fluorescent detection reagent; Eiken Chemical Co. Ltd) was added to 25 μl of LAMP products. For a positive reaction, the colour changed from orange to green, whereas a negative reaction remained orange. The colour change could be observed by the naked eye under natural light or with the aid of UV light at 365 nm. For monitoring turbidity, real-time amplification by the RT-LAMP assay was monitored by spectrophotometry, recording the optical density at 650 nm every 6 s with the help of a Loopamp Realtime Turbidimeter (LA-230; Eiken Chemical Co. Ltd) [9].
Assay validation
1. Optimal primer choice and reaction temperature conditions for the RT-LAMP assay
As shown in Figure 1A, the EBL-2 primer set amplified the NP gene using the shortest time of about 10min; therefore, this was chosen as the optimal primer set for EBOV detection of RT-LAMP (Table 1). To further optimize the amplification, reaction temperatures were compared ranging from 59 °C to 69 °C at 2 °C intervals. Ultimately, 61 °C was chosen as the optimal reaction temperature (Fig. 1B).
2. Specificity of NP detection by RT-LAMP using the artificial in vitro transcribed RNA
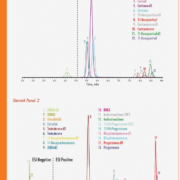
Twenty-five other non-EBOV viruses were also tested. As shown in Figure 2, the EBOV RNA was identified positively by a successful RT-LAMP reaction with EBL-2 primer set using both methods of analysis. All non-EBOV strains tested negative, including the blank control, indicating that the RT-LAMP method was specific for EBOV.
3. Sensitivity of NP detection by RT-LAMP
A 10-fold serial dilution of artificial EBOV RNA was tested by real-time turbidity monitoring (Fig. 3A), visual detection method (Fig. 3B), and qRT-PCR (Fig. 3C). The limit of detection by the visual method was 10-fold lower compared with the qRT-PCR assay.
4. Clinical sample detection
The 417 clinical blood or swab samples were analysed by RT-LAMP and qRT-PCR simultaneously. The RT-LAMP and qRT-PCR detections both showed that 307 patients were confirmed cases of EBOV infections and 106 patients tested negative for EBOV.
Summary
Zaire ebolavirus is a key member of the Filoviridae family and causes highly lethal hemorrhagic fever in human beings with extremely high morbidity and mortality. As a typical negative-sense single-stranded RNA (ssRNA) virus, EBOV possesses a nucleoprotein (NP) to facilitate genomic RNA encapsidation to form a viral ribonucleoprotein complex (RNP) together with genome RNA and polymerase, which plays the most essential role in virus proliferation cycle. EBOV is found in Central Africa, but re-emerged in Western Africa in 2014 to cause an outbreak that threatened to spread worldwide. Up until 10 January 2016, 28 601 total cases (including suspected, probable, and confirmed) and 11 300 deaths were reported in Guinea and Sierra Leone (http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html). Although several chemical agents, antibodies and vaccines are found to inhibit EBOV in animals or humans, there is no therapeutic with high efficacy that can be provided for clinical usage.
To combat the increasing incidence of EBOV infections, we developed and optimized a novel RT-LAMP assay specific for EBOV diagnosis using primers spanning the 663 bp NP sequence of the viral genome. In the RT-LAMP assay, the reverse transcription reaction and DNA amplification proceed in a single step and with incubation of the reaction mixture at a constant 61°C temperature for a given time period using a temperature-controlled water bath (or other devices that can provide a stable heat are also sufficient). Moreover, LAMP reaction primers specifically recognize five independent regions of the target sequence, compared to PCR primers that recognize two independent regions of the target sequence. The sensitivity of the PCR reaction can be greatly reduced by the presence of exogenous DNA and inhibitors. Therefore, the RT-LAMP method is more suitable for rapid detection of NP in clinical samples.
Conclusion
In conclusion, a specific, sensitive, rapid and cost effective RT-LAMP assay for NP detection in EBOV was established, which is as sensitive as other available technologies, highly specific and extremely rapid in the provision of molecular diagnosis of EBOV infections. The assay can provide accurate results in a short time frame. This makes it potentially useful for clinical diagnosis of EBOV in developing countries.
Acknowledgment
This article is based on one previously published by the authors: Li H, Wang X, Liu W, Wei X, Lin W, Li E, Li P, Dong D, Cui L, Hu X, Li B, Ma Y, Zhao X, Liu C, Yuan J. Survey and Visual detection of Zaire ebolavirus in clinical samples targeting the nucleoprotein gene in Sierra Leone. Frontiers in Microbiology 2015; 6: 1332 [10].
References
1. Frieden TR, Damon I, Bell BP, Kenyon T, Nichol S. 2014. Ebola 2014—New challenges, new global response and responsibility. N Engl J Med. 371(13): 1177–1180.
2. Hampton T. Largest-ever outbreak of Ebola virus disease thrusts experimental therapies, vaccines into spotlight. JAMA 2014; 312(10): 987–989.
3. Urgently needed: rapid, sensitive, safe and simple Ebola diagnostic tests. World Health Organization 2014. (http://www.who.int/mediacentre/news/ebola/18-november-2014-diagnostics/en/).
4. MacNeil A, Rollin PE. Ebola and Marburg hemorrhagic fevers: Neglected tropical diseases? PLoS Negl Trop Dis. 2012; 6(6): e1546.
5. Ali MT, Islam MO. A highly conserved GEQYQQLR epitope has been identified in the nucleoprotein of Ebola virus by using an in silico approach. Adv Bioinformatics 2015; 2015: 278197–278203.
6. Grolla A, Lucht A, Dick D, Strong JE, Feldmann H. Laboratory diagnosis of Ebola and Marburg hemorrhagic fever. Bull Soc Pathol Exot. 2005; 98(3):205–209.
7. Notomi T, Okayama H, Masubuchi H, Yonekawa T, Watanabe K, Amino N, Hase T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000; 28, E63.
8. Kurosaki Y, Takada A, Ebihara H, Grolla A, Kamo N, Feldmann H, Kawaoka Y, Yasuda J. Rapid and simple detection of Ebola virus by reverse transcription-loop-mediated isothermal amplification. J Virol Methods 2007; 141(1): 78–83.
9. Mori Y, Nagamine K, Tomita N, Notomi T. Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem Biophys Res Commun. 2001; 289: 150–154.
10. Li H, Wang X, Liu W, Wei X, Lin W, Li E, Li P, Dong D, Cui L, Hu X, Li B, Ma Y, Zhao X, Liu C, Yuan J. Survey and Visual detection of Zaire ebolavirus in clinical samples targeting the nucleoprotein gene in Sierra Leone. Frontiers in Microbiology 2015; 6: 1332.
The authors
Huan Li# MMed, Weishi Lin# MMed, Xuesong Wang MMed, Xiao Wei MMed, Erna Li MMed, Puyuan Li MMed, Jun Chen MMed, Silei Qi MMed, Yanyan Ma MMed, Lifei Cui MMed, Xuan Hu MMed, Xiangna Zhao PhD, Jing Yuan PhD*
Institute of Disease Control and Prevention, Academy of Military Medical Sciences, Beijing, 100071, PR China
#These authors contributed equally to this work
*Corresponding author
E-mail: yuanjing6216@163.com