Unlocking the full potential of digital pathology in routine diagnosis
The digitalization of pathology is seen as a challenging but transformative process. It is one of the fastest growing areas in healthcare and Philips Digital Pathology Solutions is a pioneer and leader in this field.
The technique creates digitalized slides from patient samples, allowing pathologists to review and share clinical data within seconds.
Digital enhances overall pathology workflow and productivity, while additionally the use of image recognition and smart software will further help pathologists to work more efficiently. It also opens up professional opportunities, globally, for remote and collaborative working. Ultimately, it has the potential to enhance patient care.
European pathology innovators like Dr Ivo van den Berghe, director of surgical pathology at the AZ Sint-Jan Bruges Hospital, Belgium, were quick to seize the initiative, understanding that digital pathology would be an enabling technology: improving patient safety, removing subjectivity and leading to new diagnostic insights.
Fundamental impact on workflow
The Bruges laboratory has a high and often challenging workload, handling around 80,000 slides a year generated by around 17,500 clinical cases. For Dr van den Berghe, the deciding factors in favour of digitalizing pathology in the clinical setting are: exceptional image quality, accuracy, measurable standardization and turnaround time. He first anticipated its impact more than eight years ago, but it was not until he began actively collaborating with Philips that his vision came to fruition. “Image, speed, quality, magnification – with Philips, they have now reached a level where we can say yes – we are there.”
The opportunity for him to instigate a complete reappraisal of the laboratory’s processes, as well as reengineering the workflow, came in 2013 when the hospital’s pathology service moved into new premises. Since then, Dr van den Berghe has worked closely with the Philips lntelliSite Pathology Solution to introduce digital pathology into routine diagnosis. “Philips could see the bigger picture from the start – and together, we have fundamentally changed the way the histopathology lab works,” he explained.
“Until now, there has been no opportunity for objectivity; pathology was therefore more of an art rather than a science. Digital pathology enables the lab to replace the subjective nature of manual slide inspection under the microscope. It enhances clinical confidence in our histopathology findings by delivering the right result first time.”
Dr van den Berghe stressed: “For our partnership to succeed, it was not simply a question of upgrading the lab’s hardware and IT. Our lab required a partner who shared our vision and would be open-minded and adaptable in understanding our changing workflow requirements. It involved matching processes and people so that they could work effectively within a modern laboratory environment.”
Philips IntelliSite Pathology Solution is an automated digital pathology image creation, management and viewing system which combines an ultra-fast scanner and image management system with dedicated software tools. The aim is to facilitate the quality of diagnosis, with the potential to allow new therapies to be developed and ultimately enhance patient care. Already available in Europe, it recently became the first global digital pathology solution marketed for primary diagnostic use in the U.S.
Confidence in results interpretation
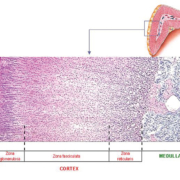
One of the most important requirements when deciding on a digital pathology solution is image quality. Dr van den Berghe explained: “If you don’t have the highest quality available, then you can’t work effectively. For something like a polyp biopsy or with chronic gastritis, that might be acceptable. However, when working with special stains, perhaps looking for mitotic figures, identifying an infiltrate or dealing with kidney tissue samples, you need the highest quality and magnification, and you need this upfront.”
Digital pathology delivers measurable levels of standardization which enhances overall quality and confidence in results. This is particularly important with the interpretation of immunohistochemistry stains. Being able to use the accuracy of whole slide imaging to determine the degree of positivity and whether to give chemotherapy or not to a patient could be very decisive in therapy. In lymphoma pathology, for instance, where typically there are numerous stains, digital pathology enables up to 10 slides to be opened in one screen so that the histopathologist can easily align them to compare different regions in the same lymph nodes. The same image can be reviewed remotely with peers.
Alongside quality, time is a critical factor. “From the moment a biopsy is taken from a patient, the clock starts ticking,” Dr van den Berghe added: “Our task is to have a turnaround time (TAT), from the biopsy to the validated report, which is as short as possible. So, the performance of the whole slide image (WSI) scanner is of equal importance. It is no use having a high quality image if you have to wait a day to see one whole slide – that won’t work.”
Scan quality, speed and performance
Delays in scanning times can also be avoided by standardizing the workflow, and reducing the need to rescan by ensuring accuracy, so that each scan is right the first time. As part of their digital pathology review process, the lab evaluated several different scanners alongside the Philips system; and identified significant discrepancies in workflow performance which could also affect TAT. If a slide’s image scan is rejected for any reason, some scanners stop operating without manual intervention, preventing further whole slide images being created and holding up workflow.
“Our scanners run overnight, so we cannot risk leaving the department and have a problem then developing which stops the scanner and the next day we arrive to find there are no slides,” said Dr van den Berghe. “With the Philips scanner, the system simply carries on.”
If the quality of one slide is flagged up for any reason, the Ultra Fast Scanner (UFS) maintains continuous production without stopping, which helps streamline overnight operation. It does not require manual corrections or rescans that may interrupt the workflow or delay a pathologist from reviewing cases. Further, it can scan one slide of 15 x 15mm tissue) within 60 seconds including the total handling time. The ease of use of the Philips scanner also helps to streamline workflow. “Very easy to use, open door, load the slides, close the door, and start – that is what a whole slide scanner should do, while delivering the highest quality and throughput possible,” he added.
Long term storage was one of the first lab processes to benefit from digitalization. The lab stores around 200,000 slides each year and ‘increased traceability and faster access without mix-ups’ has had a huge impact on overall productivity and time management. It was also helpful in enlisting staff support as the changes were implemented. “The time-saving benefits of digitalization make work less stressful for the lab technicians and there is more balance in their job, “explained Dr van den Berghe.
“As well as relying on automated traceability for stored slides, they no longer have to spend time sorting out slides by case number and by pathologist, just put the slides into the racks and load into the scanner. Our LIS automatically assigned the slides to the appropriate or subspecialist pathologist.”
Enhances multi-disciplinary collaboration
Referring to histopathology colleagues, Dr van den Berghe believes that whole slide imaging will ‘revitalize the profession’, boosting global collaboration and enhancing their diagnostic reputation. He already sees greater collaboration in the multi-disciplinary consultation meetings within the hospital, where colleagues, wherever they are based, can simply log into the system and review all the relevant patient slides. The next step will be to expand their digital platform consultancy so that the lab can add as many hospitals as possible into their consulting network, both national and international.
“I anticipate that the use of digital pathology in difficult and diagnostically rare diseases will lead to centralization of expertise through our consultancy platform, enhancing expert diagnosis. And this, at the end, will lead to the best patient care,” he confirmed.
When slides are digitized, he says, true collaboration is possible. “This is the power of digital slides. We can manage workflow and streamline everything in terms of image management, image sharing, and image analysis—simply not possible with the microscope and glass slides.”
Dr van den Berghe believes that digitalizing pathology and the resulting standardization of results will lead to more consistent, overall quality. For example, a lab can set its own parameter for an acceptable quality threshold and create a specific rule for image quality. “Any image that does not meet that predetermined measure will then automatically fail.”
New parameters for quality
However, he accepts that setting new objective parameters for quality control will have an impact on existing lab protocols, especially where decision making is still subjective. He draws specific attention to Hematoxylin & Eosin (H&E) slides and the use of their colour containers. In most labs, these are still used until someone subjectively decides that quality has started to decline. “Requiring good quality here is paramount to being confident in the results and making a positive contribution to improving outcomes. With digital pathology we need to actively discourage this subjective process,” stressed Dr van den Berghe.
Pathology plays a pivotal role in the diagnosis of disease, as well as determining and monitoring treatment. However, the need to master the manual technique of the microscope has increasingly been seen as old-fashioned and many believe it deters the next generation of recruits into the profession. “Digitizing pathology will end their reluctance,” predicts Dr van den Berghe.
When he started his journey eight years ago, he recognized that whole slide imaging could only reach its potential as part of a fully digitalized pathology workflow. Philips has created such a solution with IntelliSite. The company predicts that the digitalization of pathology will open up the sharing of clinical information with pathologists in the lab or working remotely, helping to build global networks of expertise. While their solution helps the lab satisfy demand for increased productivity, it is ultimately the patient who benefits – with faster diagnosis and enhanced outcomes.
The author
Ivo van den Berghe, MD,
Director of surgical pathology
AZ Sint-Jan Bruges Hospital, Belgium