Anti-Müllerian hormone as a biochemical marker of gonadal development and fertility status
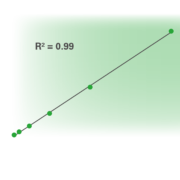
Anti-Müllerian hormone (AMH) plays a critical role in sex differentiation in fetal development and goes on to be important in the regulation of folliculogenesis in women. This article discusses the role of AMH in reproductive physiology and the many different situations where assessment of AMH levels is useful, as well as touching on methods of […]